- Record: found
- Abstract: found
- Article: found
Non-operative management of blunt hepatic and splenic injury: a time-trend and outcome analysis over a period of 17 years
Read this article at
Abstract
Background
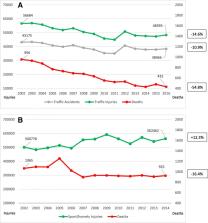
A widespread shift to non-operative management (NOM) for blunt hepatic and splenic injuries has been observed in most centers worldwide. Furthermore, many countries introduced safety measures to systematically reduce severe traffic and leisure sports injuries. This study aims to evaluate the effect of these nationwide implementations on individual patient characteristics and outcomes through a time-trend analysis over 17 years in an Austrian high-volume trauma center.
Methods
A retrospective review of all emergency trauma patients admitted to the Medical University of Innsbruck from 2000 to 2016. Injury severity, clinical data on admission, operative and non-operative treatment parameters, complications, and in-hospital mortality were evaluated.
Results
In total, 731 patients were treated with blunt hepatic and/or splenic injuries. Among these, 368 had a liver injury, 280 splenic injury, and 83 combined hepatic/splenic injury. Initial NOM was performed in 82.6% of all patients (93.5% in hepatic and 71.8% in splenic injuries) with a success rate of 96.7%. The secondary failure rate of NOM was 3.3% and remained consistent over 17 years ( p = 0.515). In terms of injury severity, we observed a reduction over time, resulting in an overall mortality rate of 4.8% and 3.5% in the NOM group (decreasing from 7.5 to 1.9% and from 5.6 to 1.3%, respectively). These outcomes confirmed an improved utilization of the NOM approach.
Conclusion
Our cohort represents one of the largest Central European single-center experiences available in the literature. NOM is the standard of care for blunt hepatic and splenic injuries and successful in > 96% of all patients. This rate was quite constant over 17 years ( p = 0.515). Overall, national and regional safety measures resulted in a significantly decreased severity of observed injury patterns and deaths due to blunt hepatic or splenic trauma. Although surgery is nowadays only applied in about one third of splenic injury patients in our center, these numbers might further decrease by intensified application of interventional radiology and modern coagulation management.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Transfusion in trauma: thromboelastometry-guided coagulation factor concentrate-based therapy versus standard fresh frozen plasma-based therapy

- Record: found
- Abstract: found
- Article: found
Splenic trauma: WSES classification and guidelines for adult and pediatric patients
- Record: found
- Abstract: found
- Article: not found