- Record: found
- Abstract: found
- Article: found
Ischemia modified albumin can act as an independent predictor of inhospital mortality in patients with acute aortic dissection
Read this article at
Abstract
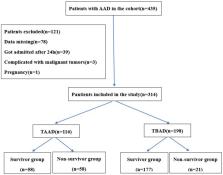
Acute aortic dissection (AAD) is a serious disease characterized by high mortality. However, there are no accurate indicators to predict in-hospital mortality. The objective of this study was to identify the potential value of ischemia modified albumin (IMA) in prediction of in-hospital mortality of AAD patients. This was a single-center, prospective study involved 314 patients undergoing AAD, including 197 males and 117 females, aged 26–87 (57.14 ± 21.71) years old, 116 cases of TAAD and 198 cases of TBAD (37 cases of complicated, 114 cases of high risk, and 47 cases of uncomplicated), 228 cases were underwent surgery/intervention treatment (77 cases of TAAD,151 cases of TBAD) and 86 cases were underwent conservative therapy (39 cases of TAAD, 47 cases of TBAD). The basic data, on-admission IMA level, and the all-cause in-hospital mortality was recorded. IMA in the non-survivor group and TAAD group was found to be significantly higher than that in the survivor group and TBAD group (P < 0.001). Multivariate logistic regression analysis results revealed that age ( OR = 1.923, 95% CI: 1.102–4.481, P = 0.020), conservative therapy ( OR = 17.892, 95% CI: 7.641–24.748, P < 0.001), D-dimer level ( OR = 3.517, 95% CI: 1.874–7.667, P = 0.011) and IMA level ( OR = 5.406, 95% CI: 2.951–10.395, P = 0.004) served as independent risk factors for in-hospital mortality of TAAD patients. And D-dimer level ( OR = 2.241, 95% CI: 1.475–5.663, P = 0.018), IMA level ( OR = 3.115, 95% CI: 1.792–6.925, P = 0.009) also served as independent risk factors for in-hospital mortality of TBAD patients, whereas surgery ( OR = 0.110, 95%CI: 0.075–0.269, P < 0.001) was the protective factor of in-hospital mortality of TAAD patients. After IMA prediction, the AUC, optimal cut-off value, sensitivity, and the specificity of in-hospital mortality of AAD patients were observed to be 0.801 (95% CI: 0.744–0.858), 86.55 U/mL, 79.1%, and 73.2%, respectively. In addition, it was found that AUC was 0.799 (95% CI: 0.719–0.880) in TAAD and 0.753 (95% CI: 0.641–0.866) in TBAD. Overall, it was concluded that on-admission IMA level acted as an independent prediction index for in-hospital mortality of AAD patients.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Acute aortic syndromes: diagnosis and management, an update
- Record: found
- Abstract: found
- Article: not found