- Record: found
- Abstract: found
- Article: found
Second-Line Tests in the Diagnosis of Adrenocorticotropic Hormone-Dependent Hypercortisolism
Read this article at
Abstract
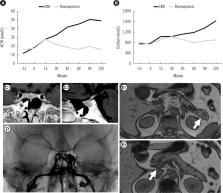
Cushing’s syndrome (CS) is a rare disease caused by chronic and excessive cortisol secretion. When adrenocorticotropin hormone (ACTH) is measurable, autonomous adrenal cortisol secretion could be reasonably ruled out in a differential diagnosis of CS. ACTH-dependent CS accounts for 80%–85% of cases and involves cortisol production stimulated by uncontrolled pituitary or ectopic ACTH secretion. Pituitary adenoma is not detected in up to one-third of cases with pituitary ACTH secretion, whereas cases of CS due to ectopic ACTH secretion may be associated with either malignant neoplasia (such as small cell lung carcinoma) or less aggressive neuroendocrine tumors, exhibiting only the typical symptoms and signs of CS. Since the differential diagnosis of ACTH-dependent CS may be a challenge, many strategies have been proposed. Since none of the available tests show 100% diagnostic accuracy, a step-by-step approach combining several diagnostic tools and a multidisciplinary evaluation in a referral center is suggested. In this review, we present a clinical case to demonstrate the diagnostic work-up of ACTH-dependent CS. We describe the most commonly used dynamic tests, as well as the applications of conventional or nuclear imaging and invasive procedures.
Related collections
Most cited references70
- Record: found
- Abstract: found
- Article: not found
Treatment of Cushing's Syndrome: An Endocrine Society Clinical Practice Guideline.
- Record: found
- Abstract: found
- Article: not found