- Record: found
- Abstract: found
- Article: found
The use of tracheal sounds for the diagnosis of sleep apnoea
Read this article at
Abstract
Tracheal sounds have been the subject of many research studies. In this review, we describe the state of the art, original work relevant to upper airways obstruction during sleep, and ongoing research concerning the methods used when analysing tracheal sounds. Tracheal sound sensors are a simple and noninvasive means of measurement and are more reliable than other breathing sensors. Developments in acoustic processing techniques and enhancements in tracheal sound signals over the past decade have led to improvements in the accuracy and clinical relevance of diagnoses based on this technology. Past and current research suggests that they may have a significant role in the diagnosis of obstructive sleep apnoea.
Key points
-
Tracheal sounds are currently a topic of significant interest but are not yet used in most routine sleep study systems.
-
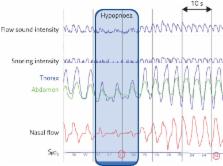
Measured at the suprasternal notch, tracheal sounds can provide reliable information on breathing sounds, snoring sounds and respiratory efforts.
-
Tracheal sounds may be used as a noninvasive method of studying abnormalities of the upper airways during wakefulness.
Educational aims
-
To understand the principles of tracheal sound measurement and analysis.
-
To highlight the importance of tracheal sounds for the diagnosis of sleep apnoea–hypopnoea syndrome.
-
To present the most relevant clinical studies that have validated the use of tracheal sound sensors and to make future clinical validation studies possible.
Abstract
Tracheal sounds analysis may have a significant role in the diagnosis of obstructive sleep apnoea http://ow.ly/f7ax30cAcnP
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group.
- Record: found
- Abstract: found
- Article: not found
The upper airway in sleep: physiology of the pharynx.
- Record: found
- Abstract: found
- Article: not found