- Record: found
- Abstract: found
- Article: found
Selection of patients for intra-arterial treatment for acute ischaemic stroke: development and validation of a clinical decision tool in two randomised trials
Read this article at
Abstract
Objective To improve the selection of patients with acute ischaemic stroke for intra-arterial treatment using a clinical decision tool to predict individual treatment benefit.
Design Multivariable regression modelling with data from two randomised controlled clinical trials.
Setting 16 hospitals in the Netherlands (derivation cohort) and 58 hospitals in the United States, Canada, Australia, and Europe (validation cohort).
Participants 500 patients from the Multicenter Randomised Clinical Trial of Endovascular Treatment for Acute Ischaemic Stroke in the Netherlands trial (derivation cohort) and 260 patients with intracranial occlusion from the Interventional Management of Stroke III trial (validation cohort).
Main outcome measures The primary outcome was the modified Rankin Scale (mRS) score at 90 days after stroke. We constructed an ordinal logistic regression model to predict outcome and treatment benefit, defined as the difference between the predicted probability of good functional outcome (mRS score 0-2) with and without intra-arterial treatment.
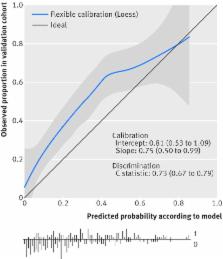
Results 11 baseline clinical and radiological characteristics were included in the model. The externally validated C statistic was 0.69 (95% confidence interval 0.64 to 0.73) for the ordinal model and 0.73 (0.67 to 0.79) for the prediction of good functional outcome, indicating moderate discriminative ability. The mean predicted treatment benefit varied between patients in the combined derivation and validation cohort from −2.3% to 24.3%. There was benefit of intra-arterial treatment predicted for some individual patients from groups in which no treatment effect was found in previous subgroup analyses, such as those with no or poor collaterals.
Conclusion The proposed clinical decision tool combines multiple baseline clinical and radiological characteristics and shows large variations in treatment benefit between patients. The tool is clinically useful as it aids in distinguishing between individual patients who may experience benefit from intra-arterial treatment for acute ischaemic stroke and those who will not.
Trial registration clinicaltrials.gov NCT00359424 (IMS III) and isrctn.com ISRCTN10888758 (MR CLEAN).
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Treating individuals 2. Subgroup analysis in randomised controlled trials: importance, indications, and interpretation.
- Record: found
- Abstract: found
- Article: not found
Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA.
- Record: found
- Abstract: found
- Article: not found