- Record: found
- Abstract: found
- Article: found
Absence of Day 3 Steroid Response Predicts Colitis-Related Complications and Colectomy in Hospitalized Ulcerative Colitis Patients
Read this article at
Abstract
Background and Aims
Rates and predictors of complications among hospitalized ulcerative colitis (UC) patients requiring high-dose corticosteroids have not been well-characterized, especially in the era of biologics.
Methods
We retrospectively studied consecutive UC admitted for a colitis flare requiring high-dose corticosteroids between April 2006 and December 2016. We evaluated rates and determinants of serious in-hospital complications (colitis-related complications, systemic complications, peri-operative complications and death) and colectomy. We performed multivariable logistic regression analysis to assess the independent association between day 3 steroid response and the risk of incurring in-hospital complications and colectomy.
Results
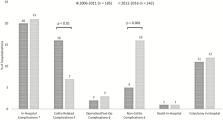
Of 427 consecutive admissions, serious in-hospital complications occurred in 87 cases (20%), while colitis-related complications occurred in 47 cases (11%). There were significantly fewer colitis-related complications during the 2012 to 2016 period as compared to the 2006 to 2011 period (7% versus 16%, P < 0.01), but significantly more systemic complications (16% versus 5%, P = 0.001). In-hospital colectomy occurred in 50 hospitalizations (12%). Day 3 steroid response was achieved in 167 hospitalizations (39%). Day 3 steroid nonresponse was significantly associated with colitis-related complications among males (adjusted odds ratio [aOR] 8.22, 95% confidence interval [CI] 1.77 to 38.17), but not among females (aOR 1.39, 95% CI 0.54 to 3.60). Older age, C. difficile infection and admission to a non-gastroenterology service were also associated with a higher risk of in-hospital complications. Day 3 steroid nonresponse was significantly associated with in-hospital colectomy (aOR 10.10, 95% CI 3.56 to 28.57).
Conclusion
In our series of UC hospitalizations for a colitis flare, absence of day 3 steroid response was associated with an increased risk of colitis-related complications among males and of in-hospital colectomy. Clinicians should recognize the importance of early steroid response as a marker to guide the need for treatment optimization.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee.
- Record: found
- Abstract: found
- Article: not found
Inflammatory bowel disease: a Canadian burden of illness review.
- Record: found
- Abstract: found
- Article: not found
