- Record: found
- Abstract: found
- Article: found
Reproducibility of a new classification of the anterior clinoid process of the sphenoid bone
Read this article at
Abstract
Background:
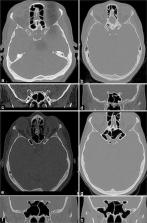
Pneumatization of the anterior clinoid process (ACP) affects paraclinoid region surgery, this anatomical variation occurs in 6.6–27.7% of individuals, making its preoperative recognition essential given the need for correction based on the anatomy of the pneumatized process. This study was conducted to evaluate the reproducibility of an optic strut-based ACP pneumatization classification by presenting radiological examinations to a group of surgeons.
Methods:
Thirty cranial computer tomography (CT) scans performed from 2013 to 2014 were selected for analysis by neurosurgery residents and neurosurgeons. The evaluators received Google Forms with questionnaires on each scan, DICOM files to be manipulated in the Horos software for multiplanar reconstruction, and a collection of slides demonstrating the steps for classifying each type of ACP pneumatization. Interobserver agreement was calculated by the Fleiss kappa test.
Results:
Thirty CT scans were analyzed by 37 evaluators, of whom 20 were neurosurgery residents and 17 were neurosurgeons. The overall reproducibility of the ACP pneumatization classification showed a Fleiss kappa index of 0.49 (95% confidence interval: 0.49–0.50). The interobserver agreement indices for the residents and neurosurgeons were 0.52 (0.51–0.53) and 0.49 (0.48–0.50), respectively, and the difference was statistically significant ( P < 0.00001).
Conclusion:
The optic strut-based classification of ACP pneumatization showed acceptable concordance. Minor differences were observed in the agreement between the residents and neurosurgeons. These differences could be explained by the residents’ presumably higher familiarity with multiplanar reconstruction software.
Related collections
Most cited references23
- Record: found
- Abstract: not found
- Book: not found
Statistical methods for rates and proportions.
- Record: found
- Abstract: found
- Article: not found
A combined epi- and subdural direct approach to carotid-ophthalmic artery aneurysms.
- Record: found
- Abstract: not found
- Article: not found