- Record: found
- Abstract: found
- Article: found
Subcutaneous Fat Necrosis of Newborn: An Atypical Presentation
letter
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Sir,
A full-term male baby weighing 3 kg born by vaginal delivery was referred at 18 h
of age with respiratory distress. There was a history of perinatal asphyxia requiring
resuscitation and meconium staining of liquor. In view of severe respiratory distress,
the baby was intubated and ventilated. Chest X-ray showed few bilateral infiltrates
suggestive of meconium aspiration syndrome. On day 4, the baby developed an erythematous
rash over the back, and by the 7th day, it progressed to violaceous induration [Figures
1 and 2] Dermatology consultation was sought, and diagnosis of cellulitis was considered.
On day 8, the infant had multiple brief episodes of convulsion managed with anticonvulsants.
Cranial USG and MRI revealed intraventricular hemorrhage and bilateral periventricular
changes consistent with perinatal hypoxia. By the 11th day, lesions progressed to
multiple red, soft, fluctuant swellings, suggesting abscess formation. The lesions
coalesced to form voluminous collection with inflamed overlying skin and surrounding
area [Figure 3]. The baby was weaned off ventilator after 48 h. CBC at admission revealed
Hb 14.9 g/dL, TLC 7200, platelets 61,000; CRP was negative. Blood counts on day 4
at manifestation of skin lesions showed drop in platelet count to 31,000 and CRP 6
mg/dl (0–8 mg/dl). Broad-spectrum antibiotics were commenced after sending blood culture
as there was concern of sepsis. Ultrasonography showed hyperechoic subcutaneous tissue.
Investigations on day 7 revealed Hb 15.2 g/dL, TLC 10,200, platelet 71,000, and quantitative
CRP 158 mg/dL. Serum calcium was 10.6 mg/dl (8.8–11 mg/dl), ionic calcium 4.8 mmol/l
(2–2.7 mmol/l), triglycerides 115 mg/dl. There was persistent thrombocytopenia on
serial blood counts. USG at this point revealed increased echogenicity of subcutaneous
fat with two loculated collections measuring 12 mm × 10 mm and 10 mm × 8 mm suggestive
of subcutaneous fat necrosis with liquefaction. Blood cultures were sterile. Large
collection necessitated needle aspiration, which was done under ultrasound guidance.
Culture yielded no growth. There was white chalky pus-like discharge from the fluctuant
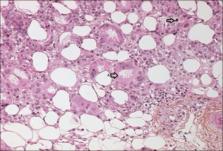
swellings for few days. Skin biopsy revealed subcutaneous tissue showing necrosis
of adipocytes and infiltration by histiocytes and mononuclear cells. Some adipocytes
showed needle-shaped clefts in radial arrangements, confirming the diagnosis of subcutaneous
fat necrosis [Figure 4]. Platelet count and CRP normalized by 3 weeks. Calcium normalized
by 4 weeks. Baby was discharged on day 34. The skin lesions regressed and complete
resolution occurred around 6 weeks with scarring. Serum calcium repeated on the last
follow-up at 3 months was normal.
Figure 1
Erythematous lesion on the back
Figure 2
Purple violaceous nodules and cystic swellings
Figure 3
Large fluctuant collections
Figure 4
Haematoxylin and eosin staining, ×400 showing A) Areas of necrosed adipocytes with
needle shaped clefts B) Lipid laden histiocytes
Subcutaneous fat necrosis is a form of benign lobular panniculitis affecting term
or post-term neonates.[1
2
4]
Leukocytosis, positive CRP, and low platelet count with cellulitis-like picture favored
the initial diagnosis of neonatal sepsis in our case. Diagnosis of SCFN was first
considered when ultrasonic evaluation revealed ill-defined areas of increased echogenicity
in the subcutaneous fat with loculated collections and normal underlying muscles.
Skin biopsy confirmed the diagnosis. USG with Doppler is a less invasive alternative
to biopsy for diagnosis and shows high echo signal with or without calcifications
and increased blood flow.[5] Possible differential diagnoses to be considered include
bacterial cellulitis, erysipelas, sclerema neonatorum, and cold panniculitis.[3] In
pyogenic abscess, the infant is often febrile or ill. SCFN can be a close mimic of
cellulitis and sepsis; the clinical picture of an otherwise well child with a history
of perinatal hypoxia is supportive. Diagnosis can be confirmed by skin biopsy showing
characteristic findings of fat necrosis, radially arranged needle-shaped crystals
in fat cells, granulomatous infiltrates composed of lymphocytes, macrophages, and
giant cells.
Clinicians should be aware of the association between SCFN and perinatal complications.
Ultrasonography and Doppler studies can help diagnose this unusual entity and preclude
unnecessary biopsy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
In the form the patient(s) has/have given his/her/their consent for his/her/their
images and other clinical information to be reported in the journal. The patients
understand that their names and initials will not be published and due efforts will
be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Subcutaneous fat necrosis of the newborn: a systematic evaluation of risk factors, clinical manifestations, complications and outcome of 16 children.
D Teillac-Hamel, E Mahé, S Hadj-Rabia … (2007)
- Record: found
- Abstract: found
- Article: not found
Subcutaneous fat necrosis as a complication of whole-body cooling for birth asphyxia.
Vikash Oza, J. Treat, Donald N. Cook … (2010)
- Record: found
- Abstract: found
- Article: not found
Subcutaneous fat necrosis of the newborn and associated hypercalcemia: A systematic review of the literature.
Nicole S. Stefanko, Beth Drolet (2019)