- Record: found
- Abstract: found
- Article: found
Quantitative three-dimensional myocardial perfusion cardiovascular magnetic resonance with accurate two-dimensional arterial input function assessment

Read this article at
Abstract
Background
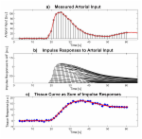
Quantification of myocardial perfusion from first-pass cardiovascular magnetic resonance (CMR) images at high contrast agent (CA) dose requires separate acquisition of blood pool and myocardial tissue enhancement. In this study, a dual-sequence approach interleaving 2D imaging of the arterial input function with high-resolution 3D imaging for myocardial perfusion assessment is presented and validated for low and high CA dose.
Methods
A dual-sequence approach interleaving 2D imaging of the aortic root and 3D imaging of the whole left ventricle using highly accelerated k-t PCA was implemented. Rest perfusion imaging was performed in ten healthy volunteers after administration of a Gadolinium-based CA at low (0.025 mmol/kg b.w.) and high dose (0.1 mmol/kg b.w.). Arterial input functions extracted from the 2D and 3D images were analysed for both doses. Myocardial contrast-to-noise ratios (CNR) were compared across volunteers and doses. Variations of myocardial perfusion estimates between volunteers and across myocardial territories were studied.
Results
High CA dose imaging resulted in strong non-linearity of the arterial input function in the 3D images at peak CA concentration, which was avoided when the input function was derived from the 2D images. Myocardial CNR was significantly increased at high dose compared to low dose, with a 2.6-fold mean CNR gain. Most robust myocardial blood flow estimation was achieved using the arterial input function extracted from the 2D image at high CA dose. In this case, myocardial blood flow estimates varied by 24 % between volunteers and by 20 % between myocardial territories when analysed on a per-volunteer basis.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
k-t PCA: temporally constrained k-t BLAST reconstruction using principal component analysis.
- Record: found
- Abstract: found
- Article: found
Quantification of myocardial perfusion by cardiovascular magnetic resonance
- Record: found
- Abstract: found
- Article: not found