- Record: found
- Abstract: found
- Article: not found
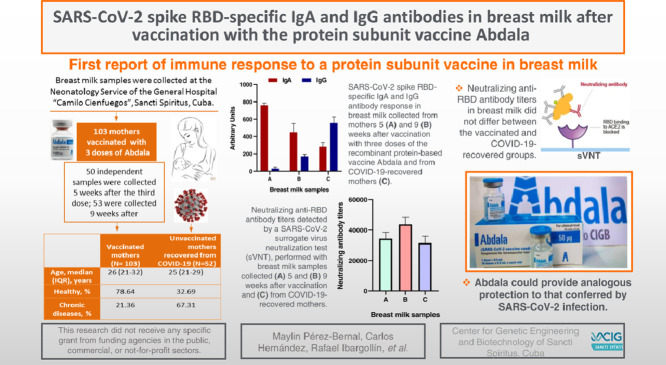
SARS-CoV-2 spike RBD-specific IgA and IgG antibodies in breast milk after vaccination with the protein subunit vaccine Abdala

Read this article at
Abstract
Background
COVID-19 vaccines that trigger a strong secretory antibody response in breast milk may achieve effective passive protection of vulnerable newborns and breastfed infants of immunized mothers. The aim of this work was to investigate the presence of SARS-CoV-2 spike RBD-specific IgA and IgG antibodies in breast milk, 5 and 9 weeks after vaccination with three doses of the protein subunit vaccine Abdala, compared to those found in breast milk from COVID-19-recovered women, collected at least 40 days after the infection.
Methods
SARS-CoV-2 spike RBD-specific IgA and IgG antibodies were semi-quantified by indirect ELISA, using a homemade standard generated by pooling twenty breast milk samples with high absorbance values according to preliminary data. The validity of the standard curves was proved following the European Medicines Agency Guideline. Two breast milk samples from two unvaccinated women who had not been infected with COVID-19 were included as negative controls. Potentially neutralizing antibodies was assessed by a SARS-CoV-2 surrogate virus neutralization test.
Results
High levels of anti-RBD IgA antibodies was detected in breast milk samples 9 weeks after vaccination and anti-RBD IgG antibodies rise from the fifth to the ninth week. In the post-COVID-19 time that was evaluated, the IgG-type response was notably higher compared to both post-vaccination periods. Neutralizing antibody titers were similar in breast milk from vaccinated and COVID-19 recovered women.
Conclusions
This is the first report about the immune response in breast milk after the administration of a COVID-19 protein subunit vaccine, which could provide analogous protection to that conferred by SARS-CoV-2 infection. This implies a potential passive immunity that breastfed infants receive from their mothers vaccinated with Abdala.
Graphical abstract
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2–spike protein–protein interaction

- Record: found
- Abstract: found
- Article: found
IgA dominates the early neutralizing antibody response to SARS-CoV-2
- Record: found
- Abstract: found
- Article: not found