- Record: found
- Abstract: found
- Article: found
Plasma PCSK9 Levels Are Elevated with Acute Myocardial Infarction in Two Independent Retrospective Angiographic Studies
Read this article at
Abstract
Objective
Proprotein convertase subtilisin/kexin type 9 (PCSK9) is a circulating protein that promotes degradation of the low density lipoprotein (LDL) receptor. Mutations that block PCSK9 secretion reduce LDL-cholesterol and the incidence of myocardial infarction (MI). However, it remains unclear whether elevated plasma PCSK9 associates with coronary atherosclerosis (CAD) or more directly with rupture of the plaque causing MI.
Methods and Results
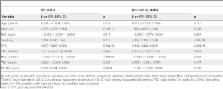
Plasma PCSK9 was measured by ELISA in 645 angiographically defined controls (<30% coronary stenosis) and 3,273 cases of CAD (>50% stenosis in a major coronary artery) from the Ottawa Heart Genomics Study. Because lipid lowering medications elevated plasma PCSK9, confounding association with disease, only individuals not taking a lipid lowering medication were considered (279 controls and 492 with CAD). Replication was sought in 357 controls and 465 with CAD from the Emory Cardiology Biobank study. PCSK9 levels were not associated with CAD in Ottawa, but were elevated with CAD in Emory. Plasma PCSK9 levels were elevated in 45 cases with acute MI (363.5±140.0 ng/ml) compared to 398 CAD cases without MI (302.0±91.3 ng/ml, p = 0.004) in Ottawa. This finding was replicated in the Emory study in 74 cases of acute MI (445.0±171.7 ng/ml) compared to 273 CAD cases without MI (369.9±139.1 ng/ml, p = 3.7×10 −4). Since PCSK9 levels were similar in CAD patients with or without a prior (non-acute) MI, our finding suggests that plasma PCSK9 is elevated either immediately prior to or at the time of MI.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Genetic and metabolic determinants of plasma PCSK9 levels.
- Record: found
- Abstract: found
- Article: not found
Dental disease and risk of coronary heart disease and mortality.
- Record: found
- Abstract: found
- Article: not found