- Record: found
- Abstract: found
- Article: found
A Comparative Study on the Effects of Postoperative 125I Brachytherapy and Irradiation After Surgical Decompression and Stabilization for Metastatic Spinal Cancers
Read this article at
Abstract
Purpose
The study aims to investigate and compare the efficacy and safety of intraoperative 125I implantation and postoperative irradiation after surgical decompression and stabilization in the treatment of patients with metastatic epidural spinal cord compression (MESCC).
Methods
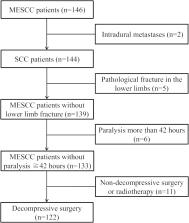
The study retrospectively enrolled 122 MESCC patients treated with surgical decompression and pedicle stabilization combined with 125I brachytherapy (the brachytherapy group) or postoperative radiotherapy (the irradiation group). Operation time, intraoperative blood loss, pain relief, postoperative ambulatory status, postoperative survival outcome, complications, and length of hospitalization were collected and compared between the two groups. Ten potential risk factors were analyzed for postoperative survival outcome.
Results
No significant difference was found in baseline characteristics between the two groups (P>0.05). Postoperative VAS score was significantly decreased, as compared with preoperative scores in both groups (P˂0.001). The VAS in the brachytherapy group was significantly lower than that in the irradiation group at postoperative 1 month, 3 months, and 6 months (P˂0.05). The postoperative ambulatory rates were 90.0% (54/60) in the brachytherapy group and 83.9% (52/62) in the irradiation group (P=0.32). The median overall survival time was similar between the two groups (7.43 months vs 7.27 months, P=0.37). Of all patients in the brachytherapy group, 25.0% (15/60) of patients suffered from complications, while 46.8% (29/62) of patients had complications in the irradiation group (P=0.0086). According to the multiple Cox regression, primary sites (P=0.038), ECOG performance status (P=0.014), and visceral metastases (P=0.0016) showed significance for postoperative survival outcome.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial.
- Record: found
- Abstract: found
- Article: not found
Metastatic epidural spinal cord compression.
- Record: found
- Abstract: found
- Article: not found