- Record: found
- Abstract: found
- Article: found
Case 4 - 84-Year old female with precordial pain and cardiac arrest with pulseless electrical activity
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
An 84-year old woman, born in Itamuji (Minas Gerais) and from São Paulo (SP), with
arterial hypertension, history of atrial fibrillation, and former smoker, has sought
for
emergency medical care due to a prolonged precordial pain (Mar 03, 2010).
The patient started medical treatment at InCor in June, 2005, when she received treatment
for arrhythmia, dyspnea on exertion and precordial pain, which occurred in prolonged
episodes, without precise triggers, during the previous six years. She was administrating
warfarin 2.5mg in alternate days and, daily doses of captopril 150mg, amiodarone 200mg,
isosorbide mononitrate 20mg, spirinolactone 25mg, metoprolol 100mg, furosemide 40mg
and
cilostazol 100mg.
ECG (Jun 24, 2005) showed atrial fibrillation rhythm, mean heart rate of 89bpm, QRS
duration 85ms, Qtc = 470 ms, SÂQRS 0º (Figure
1).
Figure 1
ECG. Atrial fibrillation
Test results (Jun 24, 2005) showed: hemoglobin 12.6 g / dL, hematocrit 39%, white
blood
cells 5.800/mm
3
, sodium 142mEq/L,
potassium 5.8mEq/L and serology to detect positive (Elisa) and negative (indirect
immunofluorescence) Chagas disease.
Physical exam (Jun 29, 2005) showed irregular 88bpm pulse rate, 150 x 110mmHg blood
pressure, symmetric pulse, pulmonary auscultation was normal, cardiac auscultaiton
showed
arrhythmic heart sounds and hyperphonesis of 2nd heart sound in aortic area. There
were no
abnormalities in the examination of abdomen and lower limbs. The following medication
was
interrupted: amiodarone, isosorbide mononitrate and cilostazol.
Two months later (August, 2005) showed large hematomas on abdomen and lower limbs,
although
INR is within the therapeutic range, 2, 32, and oral anticoagulant was interrupted
for a
period of time.
Echocardiogram (Jan, 2006) revealed left ventricle hypertrophy (11mm posterior wall
and
12mm interventricular septum), left ventricle with normal dimensions (47 x 32mm) and
normal
ejection fraction (59%); left atrium diameter was 41mm, enlargement of aortic root
diameter
(43mm) and aorta arch size was normal (28mm). Mitral annular calcification was present;
there were no valvular changes.
New ECG (Feb, 2006) revealed sinus bradycardia (43mm) (Figure 2).
Figure 2
ECG. Sinus bradycardia
Long-term electrocardiogram using Holter system (Jan 02, 2007), revealed sinus rhythm,
15
isolated ventricular extrasystoles, and 2 pairs; 2,878 atrial extrasystoles (229 pairs,
9
atrial tachycardias: the most rapid with 175bpm frequency and the longest with 15
beats).
The complaint of "chest burn" was related to atrial extrasystoles, and there were
no
changes in the ventricular repolarization.
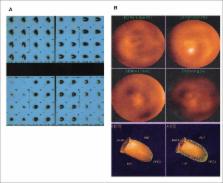
Myocardial scintigraphy with MIBI Tec99m and adenosine administration (Feb 13, 2007)
did
not indicate abnormalities on myocardial capture of the radiotracer and ejection fraction
evaluated by tomography (SPECT) was 48%, without segmental alteration of motility
(Figure 3A and Figure
3B).
Figure 3
Myocardial scintigraphy with MIBI Tec99m. 3A – normal capture; 3B ventriculography
–
LV with normal motility.
She had sought for medical care in August, 2007 due to epigastric pain and "dark colored"
vomit.
The physical exam (Aug 15, 2007) revealed revealed an eupneic and slightly pale patient
106bpm heart rate, 156 x 100mmHg blood pressure and, no other changes, except for
arrhythmic heart sounds.
Laboratory exams on that same day revealed: hemoglobin 12.7g/dL, 40% hematocrit, 8,800
white blood cells/mm
3
with normal
differential, 240,00 platelets/mm
3
, urea
86gm/dL, creatinine 1.51mg/dL, sodium 140mEq/L, potassium 5.0mEq/L, ionized calcium
1.19mmol/L, ionized magnesium 1.3mmol/L, TP (INR) 7.83, TTP (rel) 2.43, dimer-D
116ng/mL.
High digestive endoscopy (Aug 15, 2007) revealed moderate hemorrhagic erosive pangastritis
(Figure 4). Three fresh frozen plasma units were
administered, TP (INR) was recorded at 3.0 and TTP (rel) to 1.5. The patient was discharged
with proton pump inhibitor on the next day.
Figure 4
High digestive endoscopy. Moderate hemorrhagic erosive pangastritis
Laboratorial evaluation of outpatient (Apr 2008) revealed total cholesterol 235mg/dL,
HDL-c
33mg/dL, LDL-c 171mg / dL, triglycerides 156mg/dL, fasting glycemia 108mg/dL, TSH
2.09µu/mL, free T4 1.7ng/dL, sodium 144mEq/L, potassium 4.9mEq/L, urea 63mg/dL,
creatinine 1.22mg/dL and INR 2.0.
Synvastatin 40mg and digoxin 0.125mg were prescribed.
Control tests on the following year (2009) revealed total cholesterol 198mg/dL, HDL-c
36mg/dL, LDL-c96 mg/dL, triglycerides 120mg/dL, INR 2.7 and no changes on hepatic
enzymes
or creatine phosphokinase.
Long term electrocardiogram using Holter system (May 2009) revealed atrial fibrillation
rhythm with heart rate ranging from 45bpm to 143bpm. Palpitations were associated
with the
increased heart rate.
The patient progresses with occasional precordial pain and dyspnea on exertion.
She sought for medical care on the night of March 03, 2010 complaining of pain on
anterior
wall chest area, irradiating over upper limbs and abdomen, with nausea and cold sweating,
which began 3 hours earlier.
The physical examination revealed mean heart rate at 79bpm, blood pressure 127 x 91mmHg;
except for arrhythmic heart sounds, no abnormalities were reported in the physical
examination.
ECG during pain (Mar 03, 2010, 21:27) revealed atrial fibrillation rhythm, mean rate
at
121bpm, left ventricle overload and alterations on ventricular repolarization using
strain
or digital pattern (Figure 5).
Figure 5
ECG. Atrial fibrillation. Left ventricular overload with strain pattern.
ECG after the use of isosorbide (Mar 03, 2010; 22:5) showed decreased heart rate,
now at
103bpm, and onset of ST infra-unlevelling from V3 to V5 (Figure 6).
Figure 6
ECG. Atrial fibrillation and ST segment infra-unlevelling from V3 to
V5.
This led to pain relief and the administration of acetylsalicylic acid 100mg, tirofiban
0.625mg in half hour, followed by 0.33mg/h; captopril 12.5mg 8/8h and propanolol 40mg
every
8 hours.
Laboratory tests (Mar 03, 2010 at 23h) revealed hemoglobin 11.9g/dL, hematocrit 38%,
white
blood cells 9,900/mm
3
, with normal
differential, platelets 172,000/mm
3
,
total cholesterol 152mg/dL, HDL-c 35mg/dL, LDL-c 99mg/dL, triglycerides 92 mg / dl,
creatinine 1.16mg/dl (FG= 47mL/min/1.73m²), urea 58mg/dL, sodium 136mEq/L, potassium
3.8mEq/L, TP (INR) 1.8, TTPA (rel) 0.98, CK-MB mass 5.72ng/mL, troponin I below 0.2
ng /
mL, with 4-hour pain and CK-MB 5.91ng/mL with 12-h pain.
On the next morning, she had precordial pain followed by syncope and, soon after,
cardiac
arrest in pulseless electrical activity, unresponsive to resuscitation, the patient
deceased (Mar 04, 2010 at 10h30min).
Clinical Aspects
An 84-year old woman sought for medical care due to severe precordial pain. The patient
was a former smoker, had atrial fibrillation, arterial hypertension and dyslipidemia.
In
the previous six years she had long-lasting precordialgia, with more intense periods
of
pain associated with dyspnea on exertion; such episodes had led her to seek, on such
occasions, for emergency medical care.
The first diagnostic hypothesis to be considered is myocardial infarction. The main
symptom is precordial pain or discomfort, irradiation to lower limbs, jaw, shoulders
or
chest posterior area, with a duration of 20 minutes or more, associated or not with
diaphoresis, dyspnea, nausea, vomit, headache; possibly developing discomfort in the
epigastrium
1
. The patient's
symptoms support this suspicion, therefore, in addition to electrocardiogram, additional
exams were performed in order to confirm myocardial necrosis.
The patient did not have relevant alterations on CKMB, even after two dosages
2
and there was a discrete change in
troponin. However, her ECG showed infra-unlevelling of ST segment, which could suggest
ischemia of the posterior wall
1
, thus
it was chosen to administrate propanolol, isosorbide mononitrate, captopril,
acetylsalicylic acid and tirofiban.
Still, the pain frequency, present for six years, the evidence of normal ventricular
function without contraction dyskinesia in echocardiogram and myocardial scintigraphy
without ischemic alterations or presence of necrotic areas, even if carried out after
similar painful episodes, led us to alternative diagnoses.
Pulmonary thromboembolism is a probable diagnosis, since the patient had dyspnea and
mildly increased troponin level
3
, over
75 years old, history of systemic arterial hypertension, female and 4 points on
CHADS-VACS2 scoring system, which elevates her embolic risk. The presence of permanent
atrial fibrillation in oral anticoagulation with INR outside the therapeutic range
in
patient with indication for use of vitamin K antagonist also increases this
risk
4,5
.
In pulmonary thromboembolism, troponin dosage can assist in the diagnosis, being
associated with higher mortality when increased
3,6
. Another complementary
examination to be analyzed is the electrocardiogram, which, despite being unspecific
in
TEP, it may present suggestive patterns, the most common S1Q3T3 and the most common
T-wave inversion in precordial derivations of V1-V4
7
, primarily in patients with severe perfusion defect
8
, or even no electrocardiographic
changes.
The patient had a mild elevation of troponin, which would support the diagnostic
hypothesis, but not the sudden dyspnea, and her electrocardiogram does not show a
suggestive pattern, thus becoming a remote possibility.
Her elderly age, the presence of precordialgia
9
, dilation of the proximal aorta region observed in outpatient
echocardiogram associated with poorly controlled arterial hypertension, demonstrated
by
left ventricular overload in electrocardiogram and confirmed by left hypertrophy
described in the echocardiogram
10
,
increases the hypothesis of acute Stanford type A aortic dissection.
Aortic dissections are classified into Stanford type A, which corresponds to impairment
of both ascending proximal aorta and aortic arch
11
, and type B, which comprehends all other dissections, generally
dista
12
.
In people over 70 years old, the most common causes of dissection are hypertension
and
prior thoracic aneurism.
It is acknowledged that dissection mechanism occurs due to an alteration on arterial
wall caused by stress. In this case, systemic arterial hypertension is the main cause
for a reduced wall resistance, and aging is the most common reason.
The typical excruciating chest pain with irradiation to the back is uncommon in elderly
people; considering 30% of individuals with aortic dissection are treated primarily
for
other conditions, such as acute coronary syndrome, nondissecting aneurysm, pericarditis,
pulmonary thromboembolismr
13,14
.
ECG may demonstrate changes in ST segment or presence of Q-waves, since the metabolic
stress provoked by dissection in patients with atherosclerotic component may probably
cause myocardial ischemia as seen in the patient's echocardiogram
13,14
.
Syncope occurred in evolution can be related to acute pain, obstruction of brain vessels
or activation of baroreceptors
14
.
The treatment for this patient was predominantly carried out for acute coronary
syndrome; however, the administration of vasodilators, such as isosorbide mononitrate
and beta-blockers, such as propanolol, is responsible for the reduction of chrono
and
inotropism, which are important also for treatment of acute aortic dissection
2
. (Bruna Affonso Madaloso,
M.D.)
Diagnostic hypothesis: Thus, diagnoses are in descending order:
1) Acute Stanford type A aortic dissection;
2) Acute coronary syndrome - myocardial infarction;
3) Pulmonary thromboembolism (Bruna Affonso Madaloso, M.D.)
Necropsy
After opening the chest cavity, it was observed a severe pleural effusion on the left,
consisting of 1.7 liters of blood clot. There was hemorrhagic infiltration of both
pulmonary hila and adventitial hematoma at the level of distal segment of aortic arch
and proximal descending thoracic aorta. The aortic opening revealed an entry site
of
acute dissection located in the aortic isthmus, in a region of complicated
atherosclerotic plaque (Figure 7). Dissection was
progressing anterogradely throughout the aorta, extending through iliac arteries,
without detecting a re-entry orifice. There was no retrograde dissection. Severe
atherosclerosis was detected in aorta, with numerous yellowish, ulcerated plaques,
showing extensive calcification, spread throughout the vessel (Figure 8). The histological
examination of aorta confirmed acute
dissection, with cleavage in the outer third of the media; there was no inflammatory
infiltrate in the aortic wall (Figure 9). The
pericardial sac had no effusion. Cardiac examination evidenced concentric hypertrophy
of
the left ventricle, of moderate/severe level, with mild myocardial sclerosis (Figure
10). There were no infarction areas. The
macroscopic examination of epicardial coronary arteries revealed atherosclerosis with
extensive calcification areas and luminal stenosis; however, no severely obstructive
injuries. Other findings in autopsy consisted in calcification of mitral valve annulus,
renal ischemic changes, with focal areas of healed infarction, mild hepatic steatosis,
and subserosal uterine leiomyoma, measuring 1.4cm diameter. (Luiz Alberto
Benvenuti, M.D.)
Figure 7
Internal view of ascending aorta, aortic arch and beginning of descending thoracic
aorta. The entry orifice of dissection is located at the isthmus level, in
ulcerated atherosclerotic plaque (arrow). Observe the aortic wall delamination,
with presence of false lumen and adventitial hemorrhage in the initial segment of
descending thoracic aorta (asterisk).
Figure 8
Internal view of abdominal aorta evidencing severe atherosclerosis, with numerous
complicated plaques, showing ulceration and extensive calcification. Note the
aortic wall dissection, present in the distal segment of abdominal aorta
(arrow).
Figure 9
Histological section of aorta showing delamination of wall at the level of outer
third of the media, with false lumen partially filled with thrombus (arrow). Note
the presence of atherosclerotic plaque in intimal layer (asterisk).
Figure 10
Cross-section of ventricles, evidencing hypertrophy of the left ventricle, without
cavity dilation (concentric hypertrophy). Small whitish ridges visible in
myocardium correspond to myocardial sclerosis.
Anatomopathological diagnosis - Systemic atherosclerosis; concentric
hypertrophy of the left ventricle; benign nephrosclerosis; calcification of mitral
valve
annulus; uterine leiomyoma; acute dissection of aorta, ruptured to left pleural cavity
(cause of death). (Luiz Alberto Benvenuti, M.D.)
Comments
Case of a female patient, 84 years old, with systemic arterial hypertension and chronic
atrial fibrillation, who sought for emergency medical care due to prolonged precordial
pain, followed by syncope and cardiac arrest. Necropsy confirmed the hypertensive
heart
disease diagnosis in compensated phase, i.e. with left ventricle hypertrophy without
cavity dilation. Death was caused by hemothorax, secondary to acute dissection rupture
of aorta. Aorta dissection occurs when there is wall delamination, generally in the
outer third of the media, forming a false path to blood, where it penetrates through
intimal orifice. Generally it is associated with systemic arterial hypertension, such
as
in this case, but Marfan syndrome, other diseases in connective tissue, aortic valve
congenital anomalies, aorta coarctation, pregnancy or thoracic trauma may be
predisposing factors
15
. According to
DeBakey classification, the patient's dissection was type III, i.e. with entry orifice
located beyond the ascending aorta, subtype B, i.e. without retrograde dissection
of
ascending aorta. Such type of dissection (III B) corresponds to 16% of the total,
remembering that the most common is type I dissection, which entry orifice is located
in
the ascending aorta and dissection progresses to descending aorta (54% of
cases)
16
. According to Stanford
classification, dissection would be type B, i.e. without involving the ascending
aorta.
Unlike the usual, in this case, dissection occurred in aorta impaired by severe
atherosclerosis. Curiously, the entry orifice was located in an ulcerated
atherosclerotic plaque, requiring a differential diagnosis with penetrating
atherosclerotic ulcer. However, in the latter there is no true progressive dissection
of
the wall, as in this case, and lesion is localized, with possible formation of aneurysm
and local rupture
17
. (Luiz
Alberto Benvenuti, M.D.)
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease.
P. Hagan, C. A. Nienaber, E. Isselbacher … (2000)
- Record: found
- Abstract: found
- Article: not found
Prognostic value of troponins in acute pulmonary embolism: a meta-analysis.
- Record: found
- Abstract: not found
- Article: not found
Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies.
Christoph Nienaber, Kim Eagle (2003)