- Record: found
- Abstract: found
- Article: found
Management and risk factors of recurrent gestational trophoblastic neoplasia: An update from 2004 to 2017
Read this article at
Abstract
Objective
We investigated the clinical characteristics, treatments, and survival of patients with gestational trophoblastic neoplasia (GTN) who experienced recurrence. Factors predictive of recurrence were also investigated.
Methods
Patients with GTN who recurred after completing chemotherapy at Peking Union Medical College Hospital Trophoblastic Disease Center were identified between January 2004 and December 2017. Logistic regression analysis was used to identify factors predictive of GTN recurrence.
Results
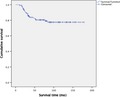
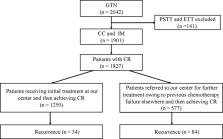
A total of 1827 patients with GTN achieved complete remission (CR) at our center, of whom 118 (6.5%) experienced recurrence during follow‐up. The recurrence rates for patients initially treated at our center and those referred to us were 2.7% and 14.6%, respectively. The majority of recurrent patients received floxuridine‐based multiagent chemotherapy (n = 64). Patients who underwent surgery achieved a significantly higher CR rate than those who did not (88.6% vs 61.1%, P = .001). Although 94.1% of recurrent patients reachieved CR, 33.3% of them recurred for a second time. The 5‐year survival rate of the entire cohort was 80.4%. An interval between antecedent pregnancy and chemotherapy >12 months (OR: 6.600, 95% CI [3.217‐13.540], P < .001), and an interval from first chemotherapy to achieving β‐human chorionic gonadotropin (β‐hCG) normalization >14 weeks (OR: 2.226, 95% CI [1.080‐4.588], P = .030) were predictors of recurrence.
Conclusions
Patients with recurrent GTN are prone to recurring for a second time. Surgery plays a beneficial role in the management of recurrent GTN. An interval between antecedent pregnancy and chemotherapy >12 months, and an interval from first chemotherapy to achieving β‐hCG normalization >14 weeks were predictors of recurrence.
Abstract
The recurrence rate for patients with gestational trophoblastic neoplasia (GTN) was 6.5%, while the re‐recurrence rate for these recurrent patients increased to 33.3%. Surgery plays a beneficial role in the management of patients with recurrent GTN. An interval between antecedent pregnancy and chemotherapy >12 months, and an interval from first chemotherapy to achieving β‐human chorionic gonadotropin normalization >14 weeks were predictors of recurrence.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Gestational trophoblastic disease II: classification and management of gestational trophoblastic neoplasia.
- Record: found
- Abstract: found
- Article: found
Pembrolizumab is effective for drug-resistant gestational trophoblastic neoplasia
- Record: found
- Abstract: found
- Article: not found