- Record: found
- Abstract: found
- Article: found
Novel non-cystic features of polycystic kidney disease: having new eyes or seeking new landscapes
Read this article at
Abstract
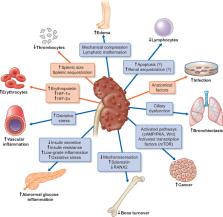
For decades, researchers have been trying to decipher the complex pathophysiology of autosomal dominant polycystic kidney disease (ADPKD). So far these efforts have led to clinical trials with different candidate treatments, with tolvaptan being the only molecule that has gained approval for this indication. As end-stage kidney disease due to ADPKD has a substantial impact on health expenditures worldwide, it is likely that new drugs targeting kidney function will be developed. On the other hand, recent clinical observations and experimental data, including PKD knockout models in various cell types, have revealed unexpected involvement of many other organs and cell systems of variable severity. These novel non-cystic features, some of which, such as lymphopenia and an increased risk to develop infections, should be validated or further explored and might open new avenues for better risk stratification and a more tailored approach. New insights into the aberrant pathways involved with abnormal expression of PKD gene products polycystin-1 and -2 could, for instance, lead to a more directed approach towards early-onset endothelial dysfunction and subsequent cardiovascular disease. Furthermore, a better understanding of cellular pathways in PKD that can explain the propensity to develop certain types of cancer can guide post-transplant immunosuppressive and prophylactic strategies. In the following review article we will systematically discuss recently discovered non-cystic features of PKD and not well-established characteristics. Overall, this knowledge could enable us to improve the outcome of PKD patients apart from ongoing efforts to slow down cyst growth and attenuate kidney function decline.
Related collections
Most cited references128
- Record: found
- Abstract: found
- Article: not found
Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study

- Record: found
- Abstract: found
- Article: found
Pathogenesis of COVID-19 from a cell biologic perspective
- Record: found
- Abstract: found
- Article: not found