- Record: found
- Abstract: found
- Article: found
Increased stomach cancer risk following radiotherapy for testicular cancer
Read this article at
Abstract
Background:
Abdominal radiotherapy for testicular cancer (TC) increases risk for second stomach cancer, although data on the radiation dose–response relationship are sparse.
Methods:
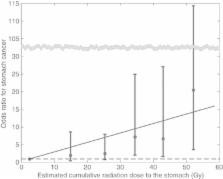
In a cohort of 22 269 5-year TC survivors diagnosed during 1959–1987, doses to stomach subsites were estimated for 92 patients who developed stomach cancer and 180 matched controls. Chemotherapy details were recorded. Odds ratios (ORs) were estimated using logistic regression.
Results:
Cumulative incidence of second primary stomach cancer was 1.45% at 30 years after TC diagnosis. The TC survivors who received radiotherapy (87 (95%) cases, 151 (84%) controls) had a 5.9-fold (95% confidence interval (CI) 1.7–20.7) increased risk of stomach cancer. Risk increased with increasing stomach dose ( P-trend<0.001), with an OR of 20.5 (3.7–114.3) for ⩾50.0 Gy compared with <10 Gy. Radiation-related risks remained elevated ⩾20 years after exposure ( P<0.001). Risk after any chemotherapy was not elevated (OR=1.1; 95% CI 0.5–2.5; 14 cases and 23 controls).
Conclusions:
Radiotherapy for TC involving parts of the stomach increased gastric cancer risk for several decades, with the highest risks after stomach doses of ⩾30 Gy. Clinicians should be aware of these excesses when previously irradiated TC survivors present with gastrointestinal symptoms and when any radiotherapy is considered in newly diagnosed TC patients.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: not found
Estimation of failure probabilities in the presence of competing risks: new representations of old estimators.
- Record: found
- Abstract: found
- Article: not found