- Record: found
- Abstract: found
- Article: found
The Swedish cause of death register
Read this article at
Abstract
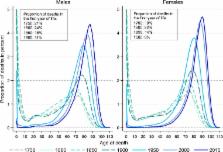
Sweden has a long tradition of recording cause of death data. The Swedish cause of death register is a high quality virtually complete register of all deaths in Sweden since 1952. Although originally created for official statistics, it is a highly important data source for medical research since it can be linked to many other national registers, which contain data on social and health factors in the Swedish population. For the appropriate use of this register, it is fundamental to understand its origins and composition. In this paper we describe the origins and composition of the Swedish cause of death register, set out the key strengths and weaknesses of the register, and present the main causes of death across age groups and over time in Sweden. This paper provides a guide and reference to individuals and organisations interested in data from the Swedish cause of death register.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Changes in rates of autopsy-detected diagnostic errors over time: a systematic review.
- Record: found
- Abstract: found
- Article: not found
Unexplained differences between hospital and mortality data indicated mistakes in death certification: an investigation of 1,094 deaths in Sweden during 1995.
- Record: found
- Abstract: found
- Article: not found