- Record: found
- Abstract: found
- Article: found
The importance of blood pressure thresholds versus predicted cardiovascular risk on subsequent rates of cardiovascular disease: a cohort study in English primary care
Summary
Background
For five decades, blood pressure lowering treatment has been recommended for patients with hypertension (currently defined as blood pressure of ≥140/90 mm Hg). In the past 20 years, guidelines for treatment began incorporating predicted absolute cardiovascular disease risk (predicted risk) and reducing blood pressure thresholds. The blood pressure threshold at which to start treatment has become a secondary consideration in some countries. We aimed to provide descriptive data to assess the relative importance of blood pressure thresholds versus predicted risk on the subsequent rate of cardiovascular disease to inform treatment decisions.
Methods
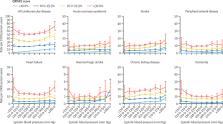
In this English population-based cohort study, we used linked data from the Clinical Practice Research Datalink (CPRD) GOLD, Hospital Episode Statistics Admitted Patient Care, and the Office for National Statistics mortality data, and area-based deprivation indices (Townsend scores). Eligible patients were aged 30–79 years on Jan 1, 2011 (cohort entry date) and could be linked to hospital, mortality, and deprivation data. Patients were followed up until death, end of CPRD follow-up, or Nov 31, 2018. We examined three outcomes: cardiovascular disease, markers of potential target organ damage, and incident dementia without a known cause. The rate of each outcome was estimated and stratified by systolic blood pressure and predicted 10-year risk of cardiovascular disease (QRISK2 algorithm).
Findings
Between Jan 1, 2011, and Nov 31, 2018, 1 098 991 patients were included in the cohort and followed up for a median of 4·3 years (IQR 2·6–6·0; total follow-up of 4·6 million person-years). Median age at entry was 52 years (IQR 42–62) and 629 711 (57·3%) patients were female. There were 51 996 cardiovascular disease events and the overall rate of cardiovascular disease was 11·2 per 1000 person-years (95% CI 11·1–11·3). Median QRISK2 10-year predicted risk was 4·6% (IQR 1·4–12·0) and mean systolic blood pressure before cohort entry was 129·1 mm Hg (SD 15·7). Within strata of predicted risk, the effect of increasing systolic blood pressure on outcomes was small. For example, in the group with 10·0–19·9% predicted risk, rates of all cardiovascular disease rose from 20·1 to 23·6 per 1000 person-years between systolic blood pressures less than 110 mm Hg and 180 and higher mm Hg. But among patients with systolic blood pressure 140·0–149·9 mm Hg, rates rose from 6·9 to 52·3 per 1000 person-years between those with less than 10·0% risk and those with 30·0% or higher predicted risk.
Interpretation
For a wide range of blood pressures, the rate of cardiovascular disease and effectiveness of blood pressure drug treatment was mainly determined by predicted risk, with blood pressure thresholds 140/90 mm Hg or 160/100 mm Hg—ubiquitous in most countries—adding little useful information. When medium-term predicted risk is low, there is no urgency to initiate drug treatment, allowing time to attempt non-pharmacological blood pressure reduction.
Related collections
Most cited references33

- Record: found
- Abstract: found
- Article: found
Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019
- Record: found
- Abstract: not found
- Article: not found
2020 International Society of Hypertension Global Hypertension Practice Guidelines
- Record: found
- Abstract: found
- Article: not found