- Record: found
- Abstract: found
- Article: found
Surgical treatment of a rare rosette-forming glioneuronal tumor in the pineal region

Read this article at
Abstract
Background:
Rosette-forming glioneuronal tumors (RGNTs) in the pineal region are rare. RGNTs have been described in the fourth ventricle, but rarely reported in other brain regions. Here, we report the radiological findings, surgical treatment, and short-term outcome of an RGNT found in the pineal region.
Case Description:
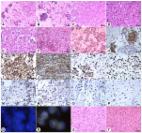
We present a case of a 22-year-old medical student with a 4-month history of headaches and diplopia. A previous magnetic resonance imaging scan revealed a mass in the pineal region, with heterogeneous contrast enhancement and hydrocephalus. Three months prior, an endoscopic biopsy and third ventriculocisternostomy were performed elsewhere; the diagnosis was neurocytoma Grade I, and radiotherapy was planned. The patient presented at our hospital for a second opinion, and we suggested surgical treatment. A near-total resection was performed in sitting position using a supracerebellar infratentorial microsurgical approach. The tumor was very soft and not well vascularized. Diplopia was initially worsened after the tumor was removed and relieved completely after 2 weeks. An 8-week follow-up examination revealed that the patient was free of symptoms. Histological analysis confirmed it was an RGNT.
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
A rosette-forming glioneuronal tumor of the fourth ventricle: infratentorial form of dysembryoplastic neuroepithelial tumor?
- Record: found
- Abstract: found
- Article: not found