- Record: found
- Abstract: found
- Article: found
Patient Activity and Survival Following Implantable Cardioverter-Defibrillator Implantation: The ALTITUDE Activity Study

Read this article at
Abstract
Background
Physical activity data are collected automatically by implantable cardioverter-defibrillators (ICDs). Though these data potentially provide a quantifiable and easily accessible measure of functional status, its relationship with survival has not been well studied.
Methods and Results
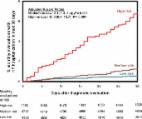
Patients enrolled in the Boston Scientific LATITUDE remote monitoring system from 2008 to 2012 with ICDs were eligible. Remote monitoring data were used to calculate mean daily activity at baseline (30 to 60 days after implantation), and longitudinally. Cox regression was used to examine the association between survival and increments of 30 minutes/day in both (1) mean baseline activity and (2) time-varying activity, with both adjusted for demographic and device characteristics. A total of 98 437 patients were followed for a median of 2.2 years (mean age of 67.7±13.1 years; 71.7% male). Mean baseline daily activity was 107.5±66.2 minutes/day. The proportion of patients surviving after 4 years was significantly higher among those in the most versus least active quintile of mean baseline activity (90.5% vs. 50.0%; log-rank P value, <0.001). Lower mean baseline activity (i.e., incremental difference of 30-minutes/day) was independently associated with a higher risk of death (adjusted hazard ratio [AHR], 1.44; 95% confidence interval [CI], 1.427 to 1.462). Time-varying activity was similarly associated with a higher risk of death (AHR, 1.48; 95% CI, 1.451 to 1.508), indicating that a patient having 30 minutes per day less activity in a given month has a 48% increased hazard for death when compared to a similar patient in the same month.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Long-term outcome after ICD and CRT implantation and influence of remote device follow-up: the ALTITUDE survival study.
- Record: found
- Abstract: found
- Article: not found
Combined heart failure device diagnostics identify patients at higher risk of subsequent heart failure hospitalizations: results from PARTNERS HF (Program to Access and Review Trending Information and Evaluate Correlation to Symptoms in Patients With Heart Failure) study.
- Record: found
- Abstract: found
- Article: found