- Record: found
- Abstract: found
- Article: found
Application of Butorphanol versus Sufentanil in Multimode Analgesia via Patient Controlled Intravenous Analgesia After Hepatobiliary Surgery: A Retrospective Cohort Study
Read this article at
Abstract
Purpose
We investigate the efficacy and safety of butorphanol in multimodal analgesia combined with dexmedetomidine and ketorolac via patient-controlled intravenous analgesia (PCIA) after hepatobiliary surgery, as compared with sufentanil.
Patients and Methods
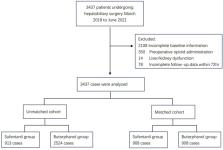
Postoperative follow-up data of hepatobiliary surgery patients in Henan Provincial People’s Hospital from March 2018 to June 2021 were collected retrospectively and divided into butorphanol group (group B) or sufentanil group (group S) according to the postoperative intravenous controlled analgesia scheme. The baseline characteristics and surgical information of the two groups were matched through propensity score matching (PSM).
Results
A total of 3437 patients were screened, and PSM yielded 1816 patients after matching, including 908 in the butorphanol group and 908 in the sufentanil group. Compared with group S, the incidence of moderate-to-severe pain on the first postoperative day and the second postoperative day was lower in group B during rest (3.2% vs 10.9%, P<0.001; 1.2% vs 4.6%, P<0.001), and during movement (7.0% vs 18.9%, P<0.001; 2.6% vs 8.7%, P<0.001). Patients receiving butorphanol had a lower morphine consumption (50mg vs 120mg, P<0.001). The bolus attempts of an analgesic pump in group B were significantly lower than in group S (1 vs 2, P<0.001). Postoperative hospital length of stay was shortened in group B (11d vs 12d, P=0.017). The occurrence of postoperative vomiting was lower in group B (1.4% vs 3.0%, P=0.025) than in group S. However, more patients in group B experienced dizziness (0.9% vs 0.1%, P=0.019).
Related collections
Most cited references53
- Record: found
- Abstract: found
- Article: not found
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration.
- Record: found
- Abstract: found
- Article: not found
Persistent postsurgical pain: risk factors and prevention.
- Record: found
- Abstract: found
- Article: not found