- Record: found
- Abstract: found
- Article: found
Telemedicine During the COVID-19 Pandemic: Impact on Care for Rare Cancers
Read this article at
Abstract
PURPOSE
Many patients with cancer, often those with rare cancers such as sarcomas, travel long distances to access expert care. The COVID-19 pandemic necessitated widespread changes in delivery of cancer care, including rapid adoption of telemedicine-based care. We aimed to evaluate the impact of telemedicine on patients, clinicians, and care delivery at the Royal Marsden Hospital (RMH) Sarcoma Unit during the pandemic.
METHODS
Data were extracted from patient records for all planned outpatient appointments at the RMH Sarcoma Unit from March 23 to April 24, 2020. Patients and clinicians completed separate questionnaires to understand their experiences.
RESULTS
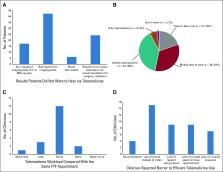
Of 379 planned face-to-face appointments, 283 (75%) were converted to telemedicine. Face-to-face appointments remained for patients who needed urgent start of therapy or performance status assessment. Patients lived on average > 1.5 hours from RMH. Patient satisfaction (n = 108) with telemedicine was high (mean, 9/10), and only 48% (n = 52/108) would not want to hear bad news using telemedicine. Clinicians found telemedicine efficient, with no associated increased workload, compared with face-to-face appointments. Clinicians indicated lack of physical examination did not often affect care provision when using telemedicine. Most clinicians (n = 17; 94%) believed telemedicine use was practice changing; congruently, 80% (n = 86/108) of patients desired some telemedicine as part of their future care, citing reduced cost and travel time.
CONCLUSION
Telemedicine can revolutionize delivery of cancer care, particularly for patients with rare cancers who often live far away from expert centers. Our study demonstrates important patient and clinician benefits; assessment of longer-term impact on patient outcomes and health care systems is needed.
Related collections
Most cited references6
- Record: found
- Abstract: found
- Article: not found
Risk of COVID-19 for patients with cancer
- Record: found
- Abstract: found
- Article: not found
Telemedicine in Cancer Care
- Record: found
- Abstract: found
- Article: not found
