- Record: found
- Abstract: found
- Article: found
Gender differences in clinical presentation and 1-year outcomes in atrial fibrillation
Read this article at
Abstract
Objectives
Our objective was to examine gender differences in clinical presentation, management and prognosis of atrial fibrillation (AF) in a contemporary cohort.
Methods
In 6412 patients, 39.7% women, of the PREvention oF thromboembolic events – European Registry in Atrial Fibrillation, we examined gender differences in symptoms, risk factors, therapies and 1-year incidence of adverse outcomes.
Results
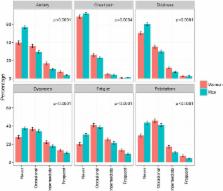
Men with AF were on average younger than women (mean±SD: 70.1±10.7 vs 74.1±9.7 years, p<0.0001). Women more frequently had at least one AF-related symptom at least occasionally compared with men (95.4% in women, 89.8% in men, p<0.0001). Prescription of oral anticoagulation was similar, with an increase of non-vitamin K antagonist oral anticoagulants from 5.9% to 12.6% in women and from 6.2% to 12.6% in men, p<0.0001 for both.
Men were more frequently treated with electrical cardioversion and ablation (20.6% and 6.3%, respectively) than women (14.9% and 3.3%, respectively), p<0.0001. Women had 65% (OR: 0.35; 95% CI (0.22 to 0.56)) lower age-adjusted and country-adjusted odds of coronary revascularisation, 40% (OR: 0.60; (0.38 to 0.93)) lower odds of acute coronary syndrome and 20% (OR: 0.80; (0.68 to 0.96)) lower odds of heart failure at 1 year. There were no statistically significant gender differences in 1-year stroke/transient ischaemic attack/arterial thromboembolism and major bleeding events.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative.

- Record: found
- Abstract: found
- Article: found
Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies

- Record: found
- Abstract: found
- Article: found