- Record: found
- Abstract: found
- Article: found
Health Center Testing for SARS-CoV-2 During the COVID-19 Pandemic — United States, June 5–October 2, 2020
research-article

Lisa Romero , DrPH
1
,
,
Leah Zilversmit Pao , PhD
1 ,
Hollie Clark , MPH
1 ,
Catharine Riley , PhD
1 ,
Sharifa Merali , MPH
1 ,
Michael Park , PhD
1 ,
Carrie Eggers , MPH
1 ,
Stephanie Campbell , MPH
2 ,
Cuong Bui
2 ,
Joshua Bolton , MS
2 ,
Xuan Le , AM
2 ,
Robyn Neblett Fanfair , MD
1 ,
Michelle Rose , PhD
1 ,
Alison Hinckley , PhD
1 ,
Charlene Siza , DVM
1
18 December 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Long-standing social inequities and health disparities have resulted in increased
risk for coronavirus disease 2019 (COVID-19) infection, severe illness, and death
among racial and ethnic minority populations. The Health Resources and Services Administration
(HRSA) Health Center Program supports nearly 1,400 health centers that provide comprehensive
primary health care* to approximately 30 million patients in 13,000 service sites
across the United States.
†
In 2019, 63% of HRSA health center patients who reported race and ethnicity identified
as members of racial ethnic minority populations (
1
). Historically underserved communities and populations served by health centers have
a need for access to important information and resources for preventing exposure to
SARS-CoV-2, the virus that causes COVID-19, to testing for those at risk, and to follow-up
services for those with positive test results.
§
During the COVID-19 public health emergency, health centers
¶
have provided and continue to provide testing and follow-up care to medically underserved
populations**; these centers are capable of reaching areas disproportionately affected
by the pandemic.
††
HRSA administers a weekly, voluntary Health Center COVID-19 Survey
§§
to track health center COVID-19 testing capacity and the impact of COVID-19 on operations,
patients, and personnel. Potential respondents can include up to 1,382 HRSA-funded
health centers.
¶¶
To assess health centers’ capacity to reach racial and ethnic minority groups at increased
risk for COVID-19 and to provide access to testing, CDC and HRSA analyzed survey data
for the weeks June 5–October 2, 2020*** to describe all patients tested (3,194,838)
and those who received positive SARS-CoV-2 test results (308,780) by race/ethnicity
and state of residence. Among persons with known race/ethnicity who received testing
(2,506,935), 36% were Hispanic/Latino (Hispanic), 38% were non-Hispanic White (White),
and 20% were non-Hispanic Black (Black); among those with known race/ethnicity with
positive test results, 56% were Hispanic, 24% were White, and 15% were Black. Improving
health centers’ ability to reach groups at increased risk for COVID-19 might reduce
transmission by identifying cases and supporting contact tracing and isolation. Efforts
to improve coordination of COVID-19 response-related activities between state and
local public health departments and HRSA-funded health centers can increase access
to testing and follow-up care for populations at increased risk for COVID-19.
HRSA administers a weekly voluntary Health Center COVID-19 Survey to track health
center COVID-19 testing capacity and the impact of COVID-19 on operations, patients,
and staff members. The 1,382 health centers asked to complete the survey are located
in all 50 states, the District of Columbia (DC), and five territories and freely associated
states.
†††
This analysis used survey data from the weeks ending June 5–October 2, 2020, to describe
the patient population and, among all patients who received testing for SARS-CoV-2
with viral tests (i.e., polymerase chain reaction and antigen tests), the numbers
and proportions of persons with tests and positive results by race/ethnicity and state
of residence. State survey response rates ranged from 68% to 80% among health centers.
Proportions of patients receiving SARS-CoV-2 tests and positive test results included
unreported race/ethnicity as a separate category.
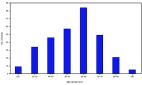
As reported in the HRSA Uniform Data System in 2019, HRSA-funded health centers reported
that 35% of their national patient population was White, 35% Hispanic,
§§§
18% Black, 4% Asian, 1% American Indian/Alaska Native (AI/AN), 1% Native Hawaiian/Other
Pacific Islander, and 1.3% multiracial persons; race/ethnicity was not reported for
6% of the patient population (Figure) (
1
). By comparison, the 2019 American Community Survey
¶¶¶
estimated that the U.S. population comprises 60% White, 18% Hispanic, 12% Black, 6%
Asian, 1% AI/AN, 0.2% Native Hawaiian/Other Pacific Islander, and 3% multiracial persons.
FIGURE
Racial/ethnic distribution of 2019 national* and Health Resources and Services Administration
(HRSA)–funded health center
†
patient populations
§
and persons who received testing and had positive SARS-CoV-2 test results
¶
— Health Center COVID-19 Survey, United States, June 5–October 2, 2020
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease
2019; HC = health center; NH/PI = Native Hawaiian/Other Pacific Islander; NH = non-Hispanic.
* Data from the 2019 American Community Survey (https://data.census.gov/cedsci/table?d=ACS%201-Year%20Estimates%20Data%20Profiles&tid=ACSDP1Y2019.
DP05&hidePreview=false). Data include non-Hispanic NH/PI (0.2%), not visible in figure
and do not include other race (0.3%). Persons with multiracial or unreported race/ethnicity
have an unreported or non-Hispanic ethnicity.
† HRSA–funded health centers include both Federally Qualified Health Centers (FQHCs)
and Health Center Program Look-Alikes (i.e, meets all Health Care Center Program requirements
but does not receive federal funding). During the COVID-19 pandemic, HRSA provided
one-time COVID-19 funding to FQHCs and Health Center Look-Alikes to purchase, administer,
and expand capacity for testing to monitor and suppress COVID-19 testing and response-related
activities.
§ HRSA 2019 Uniform Data System. https://data.hrsa.gov/tools/data-reporting/program-data/national.
¶ HRSA COVID-19 Survey, June 5–October 2, 2020. Data for the number tested or the
number tested positive are aggregated by health centers before submission and cannot
be deduplicated, which might inflate or misrepresent the number of patients tested
or who had positive test results.
The figure is a bar graph showing the racial/ethnic distribution of U.S. 2019 national
and Health Resources and Services Administration–funded health center patient populations
and persons who received testing and had positive SARS-CoV-2 test results during June
5–October 2, 2020, based on data from the Health Center COVID-19 Survey.
During June 5–October 2, 2020, health centers responding to the survey reported that
3,194,838 patients received testing and 308,780 had positive SARS-CoV-2 test results.
Compared to other jurisdictions, Texas reported the highest number of patients who
received testing (353,081; 11%), and California reported the highest number of patients
who had positive test results (46,113; 15%). Based on data reported to the Health
Center COVID-19 Survey, White and Hispanic patients each accounted for 29% of patients
who received testing for SARS-CoV-2 (Table 1) and, among patients who received positive
test results, 19% were White and 45% were Hispanic (Table 2). Overall, race was not
reported for 22% (687,903) of patients tested and 19% of patients with positive test
results (57,208); 1% (26,386) of patients receiving testing and 1% (2,378) of patients
with positive test results were multiracial. In Puerto Rico, 96% of patients receiving
testing were Hispanic; among other jurisdictions, the highest proportions of patients
receiving testing who were Hispanic were in Nevada (9,990; 56%) and New Mexico (11,705;
56%). Compared with all other jurisdictions, California reported the most Hispanic
patients who received testing (186,034) and the most positive test results among Hispanic
patients (33,310; 18%). Among those with positive test results, Puerto Rico reported
the largest proportion of Hispanic patients (2,095; 98%) and New Mexico the second
highest proportion (531; 73%). Nationally, Black patients accounted for 15% of patients
receiving testing and 12% of those who received positive test results. Mississippi
reported the highest proportion of patients who received testing who were Black (25,850;
67%) and the highest proportion of those who had positive test results who were Black
(2,348; 69%). Georgia reported the largest number of tests conducted (42,889; 43%)
and positive test results (4,204; 32%) among Black patients.
TABLE 1
Viral testing for SARS-CoV-2,* by race/ethnicity and jurisdiction
†
— Health Center COVID-19 Survey, United States, June 5–October 2, 2020
Jurisdiction
No.§ of FQHCs¶
Response range** (%)
Total no. patients tested††
Race/Ethnicity, no. tested (row %)
Hispanic/Latino
White, NH
Black, NH
Asian, NH
AI/AN, NH
NH/PI, NH
Multiracial
Unreported
United States
1,382–1,376
68–80
3,194,838
913,718 (29)
941,017 (29)
491,311 (15)
77,528 (2)
36,837 (1)
5,161 (—)
26,386 (1)
687,903 (22)
Alabama
17
59–94
46,146
3,393 (7)
16,089 (35)
21,262 (46)
183 (—)
139 (—)
4 (—)
241 (1)
4,800 (10)
Alaska
27
44–74
57,147
1,788 (3)
11,510 (20)
528 (1)
967 (2)
20,785 (36)
83 (—)
362 (1)
21,080 (37)
American Samoa
1
0–100
1,567
104 (7)
46 (3)
0 (—)
55 (4)
12 (1)
0 (—)
2 (—)
8 (1)
Arizona
23
65–83
53,455
27,220 (51)
15,584 (29)
1,509 (3)
335 (1)
1,741 (3)
50 (—)
392 (1)
6,573 (12)
Arkansas
12
50–100
51,488
7,855 (15)
24,988 (49)
13,061 (25)
243 (—)
152 (—)
21 (—)
189 (—)
4,169 (8)
California
175–178
59–74
336,454
186,034 (55)
51,114 (15)
26,371 (8)
20,103 (6)
949 (—)
634 (—)
4,891 (1)
45,217 (13)
Colorado
19
68–95
59,401
24,702 (42)
19,064 (32)
5,165 (9)
1,166 (2)
324 (1)
31 (—)
791 (1)
8,123 (14)
Connecticut
16
56–94
83,507
27,872 (33)
15,803 (19)
8,258 (10)
1,190 (1)
218 (—)
20 (—)
349 (—)
29,613 (35)
Delaware
3
33–100
2,356
894 (38)
466 (20)
850 (36)
31 (1)
9 (—)
4 (—)
14 (1)
88 (4)
District of Columbia
8
63–100
18,438
5,632 (31)
1,628 (9)
8,554 (46)
274 (1)
30 (—)
2 (—)
89 (—)
2,215 (12)
Federated States of Micronesia
4
25–100
198
0 (—)
0 (—)
0 (—)
54 (27)
0 (—)
0 (—)
0 (—)
0 (—)
Florida
47
62–87
257,119
97,542 (38)
51,704 (20)
38,483 (15)
1,868 (1)
189 (—)
44 (—)
2,431 (1)
64,665 (25)
Georgia
35
60–91
100,909
15,410 (15)
32,664 (32)
42,889 (43)
1,119 (1)
67 (—)
11 (—)
862 (1)
7,861 (8)
Guam
1
0–100
8,574
31 (—)
199 (2)
38 (—)
2,572 (30)
9 (—)
4 (—)
432 (5)
268 (3)
Hawaii
14
36–86
8,894
850 (10)
911 (10)
91 (1)
1,325 (15)
13 (—)
2,833 (32)
286 (3)
1,081 (12)
Idaho
14
71–100
12,111
3,014 (25)
6,281 (52)
168 (1)
100 (1)
1,028 (8)
25 (—)
26 (—)
1,460 (12)
Illinois
45
64–82
162,663
51,534 (32)
37,781 (23)
22,276 (14)
3,097 (2)
217 (—)
44 (—)
676 (—)
46,966 (29)
Indiana
27
48–78
20,639
6,031 (29)
5,570 (27)
2,035 (10)
967 (5)
34 (—)
3 (—)
112 (1)
5,876 (28)
Iowa
14
64–93
30,891
5,292 (17)
14,786 (48)
1,511 (5)
447 (1)
222 (1)
16 (—)
235 (1)
8,357 (27)
Kansas
19
53–100
25,472
6,582 (26)
13,631 (54)
1,972 (8)
326 (1)
336 (1)
93 (—)
212 (1)
2,264 (9)
Kentucky
25
76–96
64,494
3,453 (5)
51,839 (80)
4,141 (6)
446 (1)
36 (—)
15 (—)
506 (1)
4,017 (6)
Louisiana
36
61–81
48,007
5,297 (11)
16,396 (34)
21,333 (44)
487 (1)
143 (—)
39 (—)
323 (1)
3,968 (8)
Maine
18
50–89
9,049
600 (7)
6,614 (73)
515 (6)
40 (—)
40 (—)
7 (—)
43 (—)
1,189 (13)
Marshall Islands
1
0–100
121
0 (—)
0 (—)
0 (—)
1 (1)
0 (—)
0 (—)
0 (—)
0 (—)
Maryland
17
47–82
8,898
2,696 (30)
1,824 (20)
2,629 (30)
117 (1)
248 (3)
3 (—)
135 (2)
1,242 (14)
Massachusetts
37–38
59–89
153,411
51,639 (34)
52,813 (34)
16,444 (11)
5,326 (3)
181 (—)
61 (—)
817 (1)
25,712 (17)
Michigan
39
51–79
99,960
12,870 (13)
53,804 (54)
13,622 (14)
1,799 (2)
305 (—)
46 (—)
1,040 (1)
16,412 (16)
Minnesota
16
56–81
16,645
2,828 (17)
5,093 (31)
3,627 (22)
1,178 (7)
794 (5)
5 (—)
32 (—)
3,077 (18)
Mississippi
20
65–95
38,843
3,411 (9)
8,300 (21)
25,850 (67)
218 (1)
59 (—)
9 (—)
326 (1)
605 (2)
Missouri
28–29
66–90
78,075
7,414 (9)
36,275 (46)
16,802 (22)
677 (1)
207 (—)
57 (—)
567 (1)
15,895 (20)
Montana
14
43–86
18,377
368 (2)
7,522 (41)
31 (—)
18 (—)
441 (2)
7 (—)
60 (—)
9,928 (54)
Nebraska
7
57–86
9,224
3,585 (39)
2,167 (23)
2,008 (22)
896 (10)
40 (—)
6 (—)
97 (1)
422 (5)
Nevada
8
38–88
17,827
9,990 (56)
4,102 (23)
938 (5)
1,145 (6)
47 (—)
157 (1)
94 (1)
1,322 (7)
New Hampshire
10
70–100
3,535
936 (26)
2,140 (61)
88 (2)
80 (2)
6 (—)
3 (—)
10 (—)
272 (8)
New Jersey
23–24
33–67
51,393
26,433 (51)
9,698 (19)
7,173 (14)
603 (1)
62 (—)
43 (—)
398 (1)
6,887 (13)
New Mexico
16
75–100
20,857
11,705 (56)
4,115 (20)
295 (1)
98 (—)
1,427 (7)
12 (—)
208 (1)
2,985 (14)
New York
63
48–67
204,075
31,877 (16)
32,798 (16)
24,734 (12)
5,972 (3)
194 (—)
30 (—)
1,606 (1)
106,749 (52)
North Carolina
39
46–69
65,685
14,505 (22)
18,118 (28)
22,130 (34)
661 (1)
524 (1)
66 (—)
334 (1)
9,326 (14)
North Dakota
4
75–100
5,003
199 (4)
2,425 (48)
385 (8)
170 (3)
300 (6)
9 (—)
35 (1)
1,476 (30)
Northern Mariana Islands
1
0–100
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Ohio
51
67–82
72,400
7,604 (11)
37,561 (52)
13,461 (19)
1,216 (2)
443 (1)
39 (—)
550 (1)
11,418 (16)
Oklahoma
21
52–95
13,147
2,833 (22)
5,284 (40)
1,151 (9)
86 (1)
480 (4)
16 (—)
145 (1)
3,117 (24)
Oregon
30
73–90
17,782
6,771 (38)
7,471 (42)
474 (3)
400 (2)
686 (4)
40 (—)
145 (1)
1,697 (10)
Palau
1
0–100
1,612
0 (—)
254 (16)
4 (—)
334 (21)
0 (—)
0 (—)
0 (—)
0 (—)
Pennsylvania
43
67–91
54,143
9,563 (18)
22,464 (41)
13,911 (26)
2,549 (5)
118 (—)
13 (—)
651 (1)
4,745 (9)
Puerto Rico
21–22
73–91
28,909
27,709 (96)
134 (—)
5 (—)
0 (—)
3 (—)
0 (—)
260 (1)
798 (3)
Rhode Island
8
63–100
22,637
10,653 (47)
4,907 (22)
2,120 (9)
388 (2)
55 (—)
9 (—)
241 (1)
4,228 (19)
South Carolina
23
70–91
63,976
4,705 (7)
15,311 (24)
36,609 (57)
686 (1)
124 (—)
12 (—)
321 (1)
6,097 (10)
South Dakota
4
50–100
5,966
1,194 (20)
3,536 (59)
67 (1)
223 (4)
283 (5)
14 (—)
16 (—)
631 (11)
Tennessee
29
59–83
85,712
8,496 (10)
53,673 (63)
8,411 (10)
430 (1)
63 (—)
53 (—)
1,018 (1)
13,549 (16)
Texas
72
69–85
353,081
109,844 (31)
55,515 (16)
42,531 (12)
10,324 (3)
766 (—)
170 (—)
1,510 (—)
132,353 (37)
U.S. Virgin Islands
2
0–50
365
100 (27)
45 (12)
200 (55)
0 (—)
0 (—)
0 (—)
20 (5)
0 (—)
Utah
13
62–92
13,870
5,451 (39)
4,663 (34)
209 (2)
65 (—)
622 (4)
26 (—)
125 (1)
2,671 (19)
Vermont
11
64–100
5,017
143 (3)
4,415 (88)
42 (1)
41 (1)
16 (—)
0 (—)
10 (—)
348 (7)
Virginia
26
65–88
35,346
8,234 (23)
15,027 (43)
6,979 (20)
381 (1)
140 (—)
4 (—)
211 (1)
4,350 (12)
Washington
27
70–89
98,481
34,877 (35)
30,972 (31)
3,647 (4)
3,844 (4)
1,317 (1)
240 (—)
1,664 (2)
20,566 (21)
West Virginia
28
61–89
47,084
2,864 (6)
39,019 (83)
1,748 (4)
48 (—)
18 (—)
12 (—)
221 (—)
3,153 (7)
Wisconsin
16
69–100
23,098
10,532 (46)
4,309 (19)
1,962 (8)
153 (1)
150 (1)
15 (—)
33 (—)
5,932 (26)
Wyoming
6
33–83
1,304
559 (43)
595 (46)
14 (1)
6 (—)
25 (2)
1 (—)
22 (2)
82 (6)
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease
2019; FQHC = Federally Qualified Health Center; NH/PI = Native Hawaiian/Other Pacific
Islander; NH = non-Hispanic.
* SARS-CoV-2 viral tests include polymerase chain reaction and antigen tests.
† The Health Resources Services Administration (HRSA) funds health centers in all
50 states, the District of Columbia, and the following U.S. territories and freely
associated states: American Samoa, Federated States of Micronesia, Guam, Northern
Mariana Islands, Marshall Islands, Puerto Rico, and U.S. Virgin Islands.
§ In June 2020, the number of HRSA-fund health centers was 1,382. By September, the
number of HRSA-funded centers decreased to 1,376, by three in California and by one
each in Massachusetts, Missouri, New Jersey, and Puerto Rico. By October, the number
of Puerto Rico’s HRSA-funded health centers increased by one.
¶ FQHCs receive HRSA Health Center Program federal grant funding to improve the health
of underserved populations
** The weekly response rate was calculated using the number of health centers that
responded to the survey as the numerator and number of current HRSA-funded health
centers as the denominator. The response range represents the lowest response rate
and the highest response rate nationally and by state during June 5–October 2, 2020.
†† Data for the number of persons receiving testing or who had positive test results
are aggregated by health center before submission and cannot be deduplicated, which
might inflate or misrepresent the number of patients who received testing or who had
positive test results.
TABLE 2
Positive viral tests for SARS-CoV-2,* by race/ethnicity and jurisdiction
†
— Health Center COVID-19 Survey, United States, June 5–October 2, 2020
Jurisdiction
Total positive§
Race/Ethnicity, no. positive (row %)
Hispanic/Latino
White, NH
Black, NH
Asian, NH
AI/AN, NH
NH/PI, NH
Multiracial
Unreported
United States
308,780
140,462 (45)
59,959 (19)
38,385 (12)
6,792 (2)
1,262 (—)
473 (—)
2,378 (1)
57,208 (19)
Alabama
5,097
710 (14)
1,469 (29)
2,296 (45)
23 (—)
14 (—)
0 (—)
32 (1)
542 (11)
Alaska
961
81 (8)
167 (17)
31 (3)
18 (2)
253 (26)
0 (—)
7 (1)
399 (42)
American Samoa
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Arizona
8,297
4,719 (57)
1,857 (22)
243 (3)
25 (—)
178 (2)
9 (—)
70 (1)
1,190 (14)
Arkansas
5,946
1,808 (30)
1,738 (29)
883 (15)
14 (—)
13 (—)
7 (—)
10 (—)
886 (15)
California
46,113
33,310 (72)
4,075 (9)
2,458 (5)
997 (2)
76 (—)
63 (—)
572 (1)
4,470 (10)
Colorado
4,656
3,234 (69)
721 (15)
142 (3)
49 (1)
14 (—)
3 (—)
10 (—)
480 (10)
Connecticut
3,904
2,032 (52)
221 (6)
229 (6)
33 (1)
2 (—)
1 (—)
3 (—)
1,379 (35)
Delaware
244
144 (59)
19 (8)
71 (29)
4 (2)
2 (1)
0 (—)
0 (—)
4 (2)
District of Columbia
1,697
737 (43)
82 (5)
696 (41)
16 (1)
4 (—)
0 (—)
6 (—)
154 (9)
Federated States of Micronesia
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Florida
43,859
17,913 (41)
3,500 (8)
3,347 (8)
131 (—)
9 (—)
2 (—)
142 (—)
18,802 (43)
Georgia
13,130
2,984 (23)
4,213 (32)
4,204 (32)
69 (1)
6 (—)
2 (—)
48 (—)
1,597 (12)
Guam
633
2 (—)
5 (1)
0 (—)
222 (35)
0 (—)
0 (—)
35 (6)
2 (—)
Hawaii
907
63 (7)
27 (3)
3 (—)
144 (16)
1 (—)
234 (26)
20 (2)
78 (9)
Idaho
2,938
1,185 (40)
991 (34)
119 (4)
55 (2)
94 (3)
18 (1)
9 (—)
467 (16)
Illinois
16,752
6,993 (42)
3,571 (21)
2,074 (12)
151 (1)
16 (—)
1 (—)
55 (—)
3,874 (23)
Indiana
3,274
1,372 (42)
600 (18)
238 (7)
152 (5)
2 (—)
0 (—)
12 (—)
897 (27)
Iowa
3,634
1,011 (28)
1,550 (43)
141 (4)
68 (2)
14 (—)
1 (—)
25 (1)
821 (23)
Kansas
2,810
1,345 (48)
986 (35)
177 (6)
27 (1)
30 (1)
5 (—)
3 (—)
226 (8)
Kentucky
4,191
579 (14)
2,884 (69)
306 (7)
35 (1)
0 (—)
2 (—)
22 (1)
361 (9)
Louisiana
4,922
734 (15)
1,826 (37)
2,088 (42)
29 (1)
11 (—)
0 (—)
37 (1)
191 (4)
Maine
119
28 (24)
42 (35)
43 (36)
0 (—)
0 (—)
0 (—)
1 (1)
5 (4)
Marshall Islands
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Maryland
1,472
763 (52)
148 (10)
410 (28)
24 (2)
13 (1)
1 (—)
19 (1)
93 (6)
Massachusetts
10,029
6,755 (67)
1,167 (12)
696 (7)
312 (3)
1 (—)
1 (—)
50 (—)
1,031 (10)
Michigan
3,931
1,060 (27)
1,455 (37)
460 (12)
65 (2)
9 (—)
2 (—)
48 (1)
828 (21)
Minnesota
2,194
991 (45)
219 (10)
527 (24)
190 (9)
22 (1)
1 (—)
2 (—)
241 (11)
Mississippi
3,412
255 (7)
686 (20)
2,348 (69)
23 (1)
7 (—)
1 (—)
29 (1)
54 (2)
Missouri
5,770
1,319 (23)
2,310 (40)
1,090 (19)
48 (1)
8 (—)
0 (—)
23 (—)
916 (16)
Montana
865
26 (3)
323 (37)
2 (—)
1 (—)
30 (3)
1 (—)
2 (—)
480 (55)
Nebraska
1,749
1,171 (67)
160 (9)
138 (8)
131 (7)
2 (—)
0 (—)
6 (—)
140 (8)
Nevada
2,893
2,029 (70)
325 (11)
121 (4)
127 (4)
7 (—)
21 (1)
14 (—)
245 (8)
New Hampshire
139
91 (65)
32 (23)
8 (6)
4 (3)
0 (—)
0 (—)
0 (—)
4 (3)
New Jersey
3,275
1,080 (33)
266 (8)
287 (9)
40 (1)
0 (—)
0 (—)
16 (—)
1,584 (48)
New Mexico
729
531 (73)
89 (12)
8 (1)
2 (—)
23 (3)
0 (—)
7 (1)
66 (9)
New York
10,697
1,404 (13)
1,382 (13)
1,507 (14)
1,775 (17)
6 (—)
3 (—)
75 (1)
4,528 (42)
North Carolina
8,467
3,922 (46)
1,846 (22)
1,623 (19)
63 (1)
53 (1)
8 (—)
40 (—)
908 (11)
North Dakota
402
13 (3)
173 (43)
49 (12)
17 (4)
8 (2)
0 (—)
0 (—)
142 (35)
Northern Mariana Islands
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Ohio
4,794
1,014 (21)
1,881 (39)
1,197 (25)
88 (2)
2 (—)
21 (—)
33 (1)
556 (12)
Oklahoma
1,264
500 (40)
419 (33)
70 (6)
14 (1)
46 (4)
1 (—)
10 (1)
197 (16)
Oregon
1,785
1,011 (57)
266 (15)
79 (4)
346 (19)
14 (1)
1 (—)
3 (—)
62 (3)
Palau
0
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Pennsylvania
3,573
1,105 (31)
954 (27)
719 (20)
357 (10)
7 (—)
1 (—)
87 (2)
333 (9)
Puerto Rico
2,137
2,095 (98)
5 (—)
5 (—)
0 (—)
0 (—)
0 (—)
0 (—)
32 (1)
Rhode Island
2,808
1,943 (69)
250 (9)
196 (7)
35 (1)
0 (—)
2 (—)
19 (1)
360 (13)
South Carolina
5,399
1,087 (20)
1,075 (20)
2,602 (48)
18 (—)
18 (—)
1 (—)
16 (—)
568 (11)
South Dakota
857
167 (19)
542 (63)
5 (1)
65 (8)
18 (2)
1 (—)
1 (—)
58 (7)
Tennessee
13,014
2,726 (21)
6,116 (47)
1,544 (12)
114 (1)
22 (—)
6 (—)
432 (3)
2,038 (16)
Texas
22,444
15,079 (67)
2,588 (12)
1,725 (8)
397 (2)
47 (—)
2 (—)
180 (1)
2,419 (11)
U.S. Virgin Islands
2
0 (—)
0 (—)
2 (100)
0 (—)
0 (—)
0 (—)
0 (—)
0 (—)
Utah
1,597
1,099 (69)
284 (18)
20 (1)
6 (—)
48 (3)
1 (—)
17 (1)
116 (7)
Vermont
35
2 (6)
20 (57)
4 (11)
5 (14)
0 (—)
0 (—)
0 (—)
4 (11)
Virginia
3,966
1,684 (42)
1,272 (32)
633 (16)
23 (1)
6 (—)
0 (—)
17 (—)
331 (8)
Washington
9,601
6,115 (64)
1,295 (13)
265 (3)
219 (2)
92 (1)
39 (—)
95 (1)
1,289 (13)
West Virginia
1,792
249 (14)
1,363 (76)
78 (4)
2 (—)
0 (—)
0 (—)
8 (—)
92 (5)
Wisconsin
3,381
2,090 (62)
418 (12)
175 (5)
19 (1)
6 (—)
10 (—)
4 (—)
650 (19)
Wyoming
223
102 (46)
86 (39)
3 (1)
0 (—)
8 (4)
0 (—)
6 (3)
18 (8)
Abbreviations: AI/AN = American Indian/Alaska Native; COVID-19 = coronavirus disease
2019; NH = non-Hispanic; NH/PI = Native Hawaiian/Other Pacific Islander.
* SARS-CoV-2 viral tests include polymerase chain reaction and antigen tests.
† The Health Resources Services Administration funds health centers in all 50 states,
the District of Columbia, and the following U.S. territories and freely associated
states: American Samoa, Federated States of Micronesia, Guam, Northern Mariana Islands,
Marshall Islands, Puerto Rico, and U.S. Virgin Islands.
§ Data for the number of persons receiving testing or who had positive test results
are aggregated by health center before submission and cannot be deduplicated, which
might inflate or misrepresent the number of patients who received testing or who had
positive test results.
Discussion
Health centers’ efforts to increase testing for SARS-CoV-2 are an important mitigation
strategy to reach racial and ethnic minority groups at increased risk for COVID-19.
Published state and national data indicate that racial and ethnic minority groups
might be more likely to become infected with SARS-CoV-2, experience more severe COVID-19–associated
illness, and have higher risk for death from COVID-19 (
2
–
7
). This study contributes to understanding current health center testing patterns
and areas for improvement. Long-standing social inequalities and health disparities
among racial and ethnic minority groups likely result from a multitude of factors
that lead to increased risk for getting ill and dying of COVID-19, including discrimination,****
limited health care access and utilization, occupation, housing, and educational and
income gaps.
††††
Further, these factors might contribute to other risk factors for severe disease and
death, including limited health care access, underlying medical conditions, and higher
levels of environmental exposure. The factors contributing to disparities likely vary
widely within and among groups, depending on geographic location and other contextual
factors.
Health centers have a long-standing commitment to meeting the primary care needs of
their communities (
8
). HRSA has awarded funding
§§§§
to support health centers to purchase, administer, and expand capacity for COVID-19
testing and response-related activities, which has enabled health centers to maintain
or increase their staffing levels, conduct training, purchase personal protective
equipment, and administer tests. Health center services, including testing, contact
tracing, isolation, providing health care, and aiding recovery from the impact of
unintended negative consequences
¶¶¶¶
of mitigation strategies, have increased the capacity of health centers to reach populations
at increased risk for COVID-19 as well as access to testing and care.*****
A recent analysis of SARS-CoV-2 testing in a multistate network of health centers
during the first weeks of the COVID-19 pandemic reported small racial differences
in testing and positivity rates; however, larger differences were identified by ethnicity,
preferred language, and insurance status, underscoring health centers’ unique position
for serving racial and ethnic minority groups and addressing the ongoing need for
targeted, language-concordant testing strategies (
9
). The results of this analysis indicate that health centers have afforded racial
and ethnic minority populations access to SARS-CoV-2 testing during the COVID-19 pandemic
and that these populations were at increased risk for COVID-19, given the large percentage
of positive test results. White and Hispanic patients each accounted for 29% of tests
performed; however, only 19% of positive test results were among White persons who
received testing, whereas 61% were among racial and ethnic minority groups, with the
largest percentage of positive test results (45%) among Hispanic patients. Twenty-six
states and Puerto Rico reported >40% of positive tests among persons of Hispanic ethnicity
with 1.5% of all Hispanic patients receiving testing at Puerto Rican health centers.
The findings in this report are subject to at least five limitations. First, the data
used in this analysis are based on responses from health centers that voluntarily
reported data to the Health Center COVID-19 Survey and might not be representative
of all health centers in the United States, its territories, and freely associated
states. Second, data represent a date range of information provided by health centers
specified by weekly reporting date. Summary information across report dates is not
comparable because of differences in health center responses for a given report date.
Third, race and ethnicity data were missing for approximately 22% of patients who
received testing and 19% of patients who had positive test results. Fourth, the reported
number of patients tested each week does not fully represent the same patients included
in the reported number with positive test results that week because of a lag between
the date the specimen is collected and the availability of test results. Therefore,
positivity cannot be inferred by dividing the number of patients who received positive
test results by the number receiving testing. Finally, data for the number of persons
with testing or positive results are aggregated by health centers before submission
and cannot be deduplicated, which might inflate or misrepresent the number of patients
receiving testing or positive test results.
Health centers are an integral component of health systems designed to address structural
inequities (
10
). During the COVID-19 public health emergency, health centers have played an important
role in providing access to testing in communities disproportionately affected by
COVID-19. Health centers’ ability to reach populations at higher risk for SARS-CoV-2
infection might reduce COVID-19 transmission by identifying cases and supporting public
health contact tracing and isolation among populations they serve.
Summary
What is already known about this topic?
Long-standing social inequities and health disparities have resulted in increased
risk for COVID-19 infection, severe illness, and death among racial and ethnic minority
populations.
What is added by this report?
Health centers have provided racial and ethnic minority populations access to SARS-CoV-2
testing. Improving health centers’ ability to reach groups at increased risk for COVID-19
might reduce transmission by identifying cases and supporting contact tracing and
isolation.
What are the implications for public health practice?
Efforts to improve coordination of COVID-19 response-related activities between state
and local public health departments and HRSA-funded health centers can increase access
to testing and follow-up care for populations at increased risk for COVID-19.
Related collections
Most cited references8

- Record: found
- Abstract: found
- Article: found
Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020
Erin K. Stokes, Laura Zambrano, Kayla N. Anderson … (2020)
- Record: found
- Abstract: found
- Article: found
Characteristics and Clinical Outcomes of Adult Patients Hospitalized with COVID-19 — Georgia, March 2020
Jeremy Gold, Karen Wong, Christine Szablewski … (2020)

- Record: found
- Abstract: found
- Article: found
Characteristics Associated with Hospitalization Among Patients with COVID-19 — Metropolitan Atlanta, Georgia, March–April 2020
Marie Killerby, Ruth Link-Gelles, Sarah Haight … (2020)