- Record: found
- Abstract: found
- Article: found
Consensuses and controversies on pseudomyxoma peritonei: a review of the published consensus statements and guidelines
Read this article at
Abstract
Background
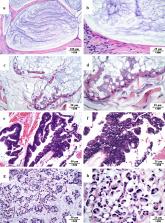
Pseudomyxoma peritonei (PMP) is a clinical malignant syndrome mainly originating from the appendix, with an incidence of 2–4 per million people. As a rare disease, an early and accurate diagnosis of PMP is difficult. It was not until the 1980s that the systematic study of this disease was started.
Main body
As a result of clinical and basic research progress over the last 4 decades, a comprehensive strategy based on cytoreductive surgery (CRS) + hyperthermic intraperitoneal chemotherapy (HIPEC) has been established and proved to be an effective treatment for PMP. Currently, CRS + HIPEC was recommended as the standard treatment for PMP worldwide. There are several consensuses on PMP management, playing an important role in the standardization of CRS + HIPEC. However, controversies exist among consensuses published worldwide. A systematic evaluation of PMP consensuses helps not only to standardize PMP treatment but also to identify existing controversies and point to possible solutions in the future. The controversy underlying the consensus and vice versa promotes the continuous refinement and updating of consensuses and continue to improve PMP management through a gradual and continuous process. In this traditional narrative review, we systemically evaluated the consensuses published by major national and international academic organizations, aiming to get a timely update on the treatment strategies of CRS + HIPEC on PMP.
Conclusion
Currently, consensuses have been reached on the following aspects: pathological classification, terminology, preoperative evaluation, eligibility for surgical treatment, maximal tumor debulking, CRS technical details, and severe adverse event classification system. However, controversies still exist regarding the HIPEC regimen, systemic chemotherapy, and early postoperative intraperitoneal chemotherapy.
Related collections
Most cited references64
- Record: found
- Abstract: found
- Article: not found