- Record: found
- Abstract: found
- Article: found
A Randomized Trial of Deep Brain Stimulation to the Subcallosal Cingulate and Nucleus Accumbens in Patients with Treatment-Refractory, Chronic, and Severe Anorexia Nervosa: Initial Results at 6 Months of Follow Up
Read this article at
Abstract
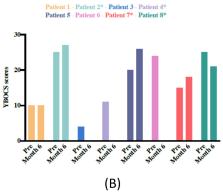
Background: The main objective of this study was to assess the safety and efficacy of deep brain stimulation (DBS) in patients with severe anorexia nervosa (AN). Methods: Eight participants received active DBS to the subcallosal cingulate (SCC) or nucleus accumbens (NAcc) depending on comorbidities (affective or anxiety disorders, respectively) and type of AN. The primary outcome measure was body mass index (BMI). Results: Overall, we found no significant difference ( p = 0.84) between mean preoperative and postoperative (month 6) BMI. A BMI reference value (BMI-RV) was calculated. In patients that received preoperative inpatient care to raise the BMI, the BMI-RV was defined as the mean BMI value in the 12 months prior to surgery. In patients that did not require inpatient care, the BMI-RV was defined as the mean BMI in the 3-month period before surgery. This value was compared to the postoperative BMI (month 6), revealing a significant increase ( p = 0.02). After 6 months of DBS, five participants showed an increase of ≥10% in the BMI-RV. Quality of life was improved ( p = 0.03). Three cases presented cutaneous complications. Conclusion: DBS may be effective for some patients with severe AN. Cutaneous complications were observed. Longer term data are needed.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
Deep brain stimulation: current challenges and future directions
- Record: found
- Abstract: found
- Article: not found
The outcome of anorexia nervosa in the 20th century.
- Record: found
- Abstract: found
- Article: not found