- Record: found
- Abstract: found
- Article: found
Type 1 Diabetes Through the Life Span: A Position Statement of the American Diabetes Association
review-article
12 June 2014
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Type 1 diabetes is characterized by an immune-mediated depletion of β-cells that results
in lifelong dependence on exogenous insulin. While both type 1 and type 2 diabetes
result in hyperglycemia, the pathophysiology and etiology of the diseases are distinct
and require us to consider each type of diabetes independently. As such, this position
statement summarizes available data specific to the comprehensive care of individuals
with type 1 diabetes. The goal is to enhance our ability to recognize and manage type
1 diabetes, to prevent its associated complications, and to eventually cure and prevent
this disease.
Incidence and Prevalence of Type 1 Diabetes
The exact number of individuals with type 1 diabetes around the world is not known,
but in the U.S., there are estimated to be up to 3 million (1). Although it has long
been called “juvenile diabetes” due to the more frequent and relatively straightforward
diagnosis in children, the majority of individuals with type 1 diabetes are adults.
Most children are referred and treated in tertiary centers, where clinical data are
more readily captured. The SEARCH for Diabetes in Youth study estimated that, in 2009,
18,436 U.S. youth were newly diagnosed with type 1 diabetes (12,945 non-Hispanic white,
3,098 Hispanic, 2,070 non-Hispanic black, 276 Asian-Pacific Islander, and 47 American
Indian) (2). Worldwide, ∼78,000 youth are diagnosed with type 1 diabetes annually.
Incidence varies tremendously among countries: East Asians and American Indians have
the lowest incidence rates (0.1–8 per 100,000/year) as compared with the Finnish who
have the highest rates (>64.2 per 100,000/year) (3). In the U.S., the number of youth
with type 1 diabetes was estimated to be 166,984 (4).
The precise incidence of new-onset type 1 diabetes in those over 20 years of age is
unknown. This may be due to the prolonged phase of onset and the subtleties in distinguishing
the different types of diabetes. In one European study of adults aged 30–70 years,
∼9% tested positive for GAD antibodies (GADA) within 5 years of a diabetes diagnosis,
consistent with other studies (5).
Adults with type 1 diabetes often receive care in primary care settings rather than
with an endocrinologist. Unlike the consolidated care seen in pediatric diabetes management,
the lack of consolidated care in adults makes incidence and prevalence rates difficult
to characterize, and therefore they are often underestimated. The number of adults
living with type 1 diabetes is increasing due to two factors: 1) the rising number
of new-onset cases of type 1 diabetes in adults, including those diagnosed with latent
autoimmune diabetes in adults (LADA), and 2) individuals with childhood-onset diabetes
are living longer (6,7).
Classification and Diagnosis
Type 1 diabetes has traditionally been diagnosed based on clinical catabolic symptoms
suggestive of insulin deficiency: polyuria, polydipsia, weight loss, and marked hyperglycemia
that is nonresponsive to oral agents. It is classified as an autoimmune disease with
progressive β-cell destruction, resulting in a physiological dependence on exogenous
insulin. Recent studies have broadened our understanding of the disease, but have
made diagnosis more complex.
There is tremendous variability in the initial presentation of type 1 diabetes in
both youth and adults. Children often present acutely, with severe symptoms of polyuria,
polydipsia, and ketonemia. However, in adults, type 1 diabetes presents with a more
gradual onset, with a clinical presentation that may initially appear consistent with
type 2 diabetes. Distinguishing between type 1 and type 2 diabetes presents diagnostic
challenges. Traditionally, progressive β-cell destruction has been the hallmark of
type 1 diabetes, but residual C-peptide (a surrogate marker for insulin secretion)
may be detected over 40 years after initial diagnosis, regardless of whether the initial
diagnosis was made in childhood or in adulthood (8).
Clinical Clues
Much of the diagnosis will depend on clinical clues, but the rising incidence of overweight/obesity
has also confounded the diagnosis of type 1 diabetes. A lean individual presenting
with clinical symptoms without a first-degree relative with diabetes (but often with
a history of distant relatives with type 1 diabetes or other autoimmune disease) is
generally suggestive of type 1 diabetes. An overweight individual (of any age) with
metabolic syndrome and a strong family history of type 2 diabetes may be assessed
only for the development of type 2 diabetes, even though type 1 diabetes is on the
differential diagnosis. Obesity does not preclude that autoimmunity and hyperglycemia
will occur even amid the relatively higher levels of endogenous insulin secretion
observed in obesity. In young patients aged 10–17 years with phenotypic type 2 diabetes,
10% have evidence of islet autoimmunity suggesting that type 1 diabetes was the likely
diagnosis (9). Thus, although leaner individuals are more likely to be diagnosed as
having type 1 diabetes, the potential for type 1 diabetes exists in those who phenotypically
appear to have type 2 diabetes. If hyperglycemia persists after treatment with noninsulin
agents, which is unusual in the treatment of newly diagnosed type 2 diabetes, then
type 1 diabetes should be considered.
Pancreatic Autoantibodies
Pancreatic autoantibodies are characteristic of type 1 diabetes. Highly sensitive
laboratory measurements capture ∼98% of individuals with autoantibodies at diagnosis
(10). Unfortunately, most commercial laboratories do not have reliably sensitive or
specific assays that measure all five autoantibodies: GADA, islet cell antibodies
(ICA), insulin autoantibodies (IAA), protein tyrosine phosphatase antibodies (ICA512
or IA2A), and zinc transporter protein (ZnT8). Thus, it may be inappropriate to report
a patient as autoantibody negative. Another cause of “false-negative” autoantibodies
is testing far out from diagnosis as antibody titers diminish over time (Fig. 1).
It appears that there is an increased incidence of type 1 diabetes in ethnic populations
where autoantibody markers may be of variable utility, such as in Asians where autoantibodies
are often negative (11–15).
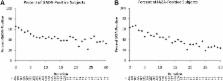
Figure 1
The percentage of antibody-positive subjects is affected by the duration of type 1
diabetes for GADA (A) and IA2A (B). Given an increase in the scatter (due to lower
numbers of subjects), the x-axis is truncated at a duration of 30 years. Reproduced
with permission from Tridgell et al. (16).
Family History
Type 1 diabetes has a genetic predilection and, in some cases, can be predicted in
family members. The overall prevalence of type 1 diabetes in the U.S. is ∼0.3%, but
if a first-degree relative has diabetes, the empiric risk of being affected is ∼5%
(17,18), representing a 15-fold increase among family members. Studies evaluating
children at risk for developing type 1 diabetes have shown that the presence of more
than two autoantibodies was associated with a nearly 70% risk for disease development
within 10 years and 84% within 15 years (19). Evaluating at-risk individuals in the
clinical setting is not yet recommended due to limited clinical interventions; however,
ongoing research studies are identifying at-risk individuals through genetic testing
in both the lower-risk general population and in the higher-risk population of relatives
of people with type 1 diabetes.
Recommendations
Diagnosis
The American Diabetes Association’s (ADA’s) diagnostic criteria for type 1 and type
2 diabetes are the same (Table 1). (A)
Consider measurement of pancreatic autoantibodies to confirm the diagnosis of type
1 diabetes. (B)
Table 1
Criteria for the diagnosis of diabetes
A1C ≥6.5%. The test should be performed in a laboratory using a method that is NGSP
certified and standardized to the DCCT assay.*
OR
FPG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least
8 h.*
OR
Two-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance
test. The test should be performed as described by the World Health Organization,
using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved
in water.*
OR
In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random
plasma glucose ≥200 mg/dL (11.1 mmol/L).
*
In the absence of unequivocal hyperglycemia, result should be confirmed by repeat
testing.
Identification of At-Risk Relatives
Inform type 1 diabetic patients of the opportunity to have their relatives tested
for type 1 diabetes risk in the setting of a clinical research study. (B)
Initial Evaluation and Follow-up
General Considerations
All patients with type 1 diabetes need age-appropriate care, with an understanding
of their specific needs and limitations. Infants and toddlers are approached quite
differently from adolescents; the needs of young adults may vary from middle-aged
or older adults. Regardless of age, the patient’s needs are the same: an individualized
care plan with ongoing education and support, ongoing assessment for acute and chronic
complications, and access to medical providers with type 1 diabetes expertise. Just
as patients change, the therapeutic approach should change and should be evaluated
at each visit and modified as needed.
Type 1 diabetes care must be an iterative process, adapted as the needs of the individual
evolve. Clinical assessments for type 1 diabetes in children and adults should incorporate
age-appropriate and complication-focused evaluations, based on the likelihood that
an abnormality will be present. For example, a young adult with low cardiovascular
disease (CVD) risk and no complications may need more of an assessment of lifestyle
adjustment as opposed to an older adult with longer duration of the disease who may
need more evaluation of vascular and neurological issues.
Transition of Care From Pediatric to Adult Providers
As youth transition into emerging adulthood, the supportive infrastructure often abruptly
disappears and glycemic control tends to deteriorate. The ADA recognizes that this
is a challenging time and recommends a strong, practical transition plan to anticipate
the upcoming changes. A successful transition plan should be initiated early (e.g.,
early teenage years) and include ongoing dialogue between the family and youth. The
discussion should include finances, insurance, obtainment of supplies, identification
of an adult care provider (ideally with communication between the two providers),
psychosocial issues (e.g., depression), and other issues identified by the family/youth.
Health care providers, family, and youth should agree to an achievable diabetes management
plan and provide resources for unanticipated issues. We refer the reader to the ADA’s
position statement on diabetes care for emerging adults (20).
Table 2 provides the childhood developmental phases and needs. Tables 3, 4, and 5
provide detailed elements of the initial and follow-up evaluation in individuals with
type 1 diabetes.
Table 2
Major developmental issues and their effect on diabetes in children and adolescents
Developmental stages (ages)
Normal developmental tasks
Type 1 diabetes management priorities
Family issues in type 1 diabetes management
Infancy (0–12 months)
Developing a trusting relationship or bond with primary caregiver(s)
Preventing and treating hypoglycemia
Coping with stress
Avoiding extreme fluctuations in blood glucose levels
Sharing the burden of care to avoid parent burnout
Toddler (13–26 months)
Developing a sense of mastery and autonomy
Preventing hypoglycemia
Establishing a schedule
Avoiding extreme fluctuations in blood glucose levels due to irregular food intake
Managing the picky eater
Limit-setting and coping with toddler’s lack of cooperation with regimen
Sharing the burden of care
Preschooler and early elementary school (3–7 years)
Developing initiative in activities and confidence in self
Preventing hypoglycemia
Reassuring child that diabetes is no one’s fault
Coping with unpredictable appetite and activity
Educating other caregivers about diabetes management
Positively reinforcing cooperation with regimen
Trusting other caregivers with diabetes management
Older elementary school (8–11 years)
Developing skills in athletic, cognitive, artistic, and social areas
Making diabetes regimen flexible to allow for participation in school or peer activities
Maintaining parental involvement in insulin and blood glucose management tasks while
allowing for independent self-care for special occasions
Consolidating self-esteem with respect to the peer group
Child learning short- and long-term benefits of optimal control
Continuing to educate school and other caregivers
Early adolescence (12–15 years)
Managing body changes
Increasing insulin requirements during puberty
Renegotiating parent and teenager’s roles in diabetes management to be acceptable
to both
Developing a strong sense of self-identity
Diabetes management and blood glucose control becoming more difficult
Learning coping skills to enhance ability to self-manage
Weight and body image concerns
Preventing and intervening in diabetes-related family conflict
Monitoring for signs of depression, eating disorders, and risky behaviors
Later adolescence (16–19 years)
Establishing a sense of identity after high school (decisions about location, social
issues, work, and education)
Starting an ongoing discussion of transition to a new diabetes team (discussion may
begin in earlier adolescent years)
Supporting the transition to independence
Integrating diabetes into new lifestyle
Learning coping skills to enhance ability to self-manage
Preventing and intervening with diabetes-related family conflict
Monitoring for signs of depression, eating disorders, and risky behaviors
Table 3
Medical history
Age and characteristics of onset of diabetes (e.g., DKA, asymptomatic laboratory finding)
Eating patterns, physical activity habits, nutritional status, and weight history
Whether or not patient wears medical alert identification
Diabetes education history; health literacy assessment
Review of previous insulin treatment regimens and response to therapy (A1C records),
treatment preferences, and prior difficulty with therapies
Current treatment of diabetes, including medications and medication adherence, meal
plan, physical activity patterns, and readiness for behavior change
Use of insulin, insulin pumps, carbohydrate ratios, and corrections; knowledge of
sick-day rules; ketone testing; pump troubleshooting (if applicable)
Results of glucose monitoring, including SMBG and CGM and patient’s use of data
DKA frequency, severity, and cause
Hypoglycemic episodes
Hypoglycemia unawareness
Any severe hypoglycemia: frequency and cause
Whether or not patient has glucagon available and someone to administer it
History of diabetes-related complications
Microvascular: retinopathy, nephropathy, and neuropathy (sensory, including history
of foot lesions; autonomic, including sexual dysfunction and gastroparesis)
Macrovascular: coronary heart disease, cerebrovascular disease, and peripheral artery
disease
Other: dental disease
Psychosocial issues, including current or past history of depression, anxiety, eating
disorders, and others; assess support systems and need for assistance
History of pregnancy and any diabetes-related complications; desire for future pregnancies
Contraception (if a woman is of childbearing age)
Smoking
Alcohol use, abuse, and impact on blood glucose levels
Illicit drug use
Driving
Table 4
Children and adolescents*
Clinical evaluation
Initial
Annual
Quarterly follow-up
Height
X
X
X
Weight
X
X†
X†
BMI percentile
X
X
X
Blood pressure
X
X
X
General physical exam
X
X
Thyroid exam
X
X
X
Injection/infusion sites
X (if already on insulin)
X
X
Comprehensive foot exam‡
If needed, based on age
Beginning with older teens with diabetes since childhood
Visual foot exam
X
If needed, based on high-risk characteristics
Retinal exam by eye care specialist
X§
In some cases, may be done every 2 years (see ADA Standards of Care)
Depression screen
X
X
X
Hypoglycemia assessment
X
X
X
Diabetes self-management skills
X
X
X
Physical activity assessment
X
X
X
Assess clinically relevant issues (e.g., alcohol, drug, and tobacco use; use of contraception;
driving)
X
As needed for teens
As needed for teens
Nutritional knowledge
X
X
As needed
Query for evidence of other autoimmune disease
X
As needed
As needed
Immunizations as recommended by CDC
X
X
As needed
Laboratory assessments
Initial
Annual
Follow-up
A1C
X
X
Every 3 months
Creatinine clearance/estimated glomerular filtration rate
X
X
Lipid panel||
Once glycemia is stable
X
As needed based on treatment
TSH
X
X
As needed based on treatment
Frequency of testing varies based on clinical symptoms, presence of antibodies, and/or
if on treatment
Antithyroid antibodies (antithyroid peroxidase and antithyroglobulin antibodies)
X
Repeat as clinically indicated
Frequency of testing is unknown; test if symptoms are present or for periodic screening
Celiac antibody panel
X
Repeat as clinically indicated
Frequency of testing is unknown; test if symptoms are present or for periodic screening
Urine albumin-to-creatinine ratio
Starting 5 years after diagnosis
X
As needed based on treatment
Islet cell antibodies: GADA/IA2A/IAA/ZnT8
X
May be needed in new-onset patients to establish diagnosis
C-peptide levels
X
Occasionally needed to establish type 1 diabetes in a patient on insulin or to verify
type 1 diabetes for insurance purposes—always measure a simultaneous blood glucose
level
*
Assumes a patient has a health care provider to manage the nondiabetes-related health
assessments and to perform annual evaluations.
†
Patient may opt out of measurement if psychologically distressing.
‡
Foot inspection should be done at each visit and self-exams taught if high-risk characteristics
are present. Comprehensive foot exam includes inspection, palpation of dorsalis pedis
and posterior tibial pulses, presence or absence of patellar and Achilles reflexes,
and determination of proprioception, vibration, and monofilament sensation.
§
Within 5 years after diagnosis.
||
If triglycerides are elevated in a nonfasting specimen, measure a direct LDL cholesterol
level.
Table 5
Adults*
Clinical evaluation
Initial
Annual
Follow-up
Height
X
Weight
X
X†
X†
BMI
X
X
Blood pressure
X
X
X
General physical exam
X
Thyroid exam
X
If indicated
Injection/infusion sites
X
X
X
Comprehensive foot exam‡
X
X
Visual foot exam
As needed—at each visit, if high-risk foot
Retinal exam by eye care specialist§
Starting 5 years after diagnosis; earlier if visual symptoms and/or true date of diagnosis
is unknown
In some individuals, screening may be done every 2 years (see ADA Standards of Medical
Care)
Depression screen
X
X
Hypoglycemia assessment
X
X
X
Diabetes self-management skills
X
X
X
Physical activity assessment
X
X
X
Assess clinically relevant issues (e.g., alcohol, drug, and tobacco use; use of contraception;
driving)
X
As needed
As needed
Nutritional knowledge
X
X
As needed
Query for evidence of other autoimmune disease
X
As needed based on clinical scenario
As needed based on clinical scenario
Immunizations as recommended by CDC
X
X
As needed
Laboratory assessments
Initial
Annual
Follow-up
A1C
X
X
Every 3 months
Creatinine clearance/estimated glomerular filtration rate
X
X
Fasting lipid panel||
X
X
As needed based on treatment
TSH
X
X
As needed based on treatment
Frequency of testing varies based on clinical symptoms, presence of antibodies, or
if on treatment
Antithyroid antibodies
X
Frequency of testing is unknown; test if symptoms are present or for periodic screening
Celiac antibody panel
X
Frequency of testing is unknown; test if symptoms are present or for periodic screening
Urine albumin-to-creatinine ratio
X
X
GADA
X
May be needed in new-onset patients to establish diagnosis
C-peptide levels
X
Occasionally needed to establish type 1 diabetes in a patient on insulin or to verify
type 1 diabetes for insurance purposes—always measure a simultaneous blood glucose
level
*
Assumes a patient has a health care provider to manage the nondiabetes-related health
assessments and to perform annual evaluations.
†
Patient may opt out of measurement if psychologically distressing.
‡
Foot inspection should be done at each visit and self-exams taught if high-risk characteristics
are present. Comprehensive foot exam includes inspection, palpation of dorsalis pedis
and posterior tibial pulses, determination of presence or absence of patellar and
Achilles reflexes, and determination of proprioception, vibration, and monofilament
sensation.
§
In some instances, the test may not need to be done yearly.
||
If a patient is unable to undertake a fasting test due to hypoglycemia, measure a
direct LDL cholesterol level.
Assessing the history of acute complications (e.g., severe hypoglycemia/hyperglycemia
and diabetic ketoacidosis [DKA]) is important. Providers should provide continuing
education for the patient/family to prevent ongoing recurrence. For example, it is
important to review exercise management to reduce hypoglycemia risk and discuss sick-day
management to reduce DKA risk.
Risk factor (e.g., cardiovascular) evaluation for prevention and screening for early
evidence of micro- and macrovascular complications for early intervention should be
implemented starting in adolescence and continue through adulthood. For children,
risk factors should be assessed shortly after diagnosis based on family history and
initial screening laboratory test results. Providers should manage risk factors, considering
age-specific goals and targets (e.g., blood pressure, lipid, depression, and BMI assessment
and management). The frequency of ongoing screening for complications should be based
on age and disease duration.
Coexistent Autoimmunity
Celiac Disease
Celiac disease is an immune-mediated disorder that occurs with increased frequency
in patients with type 1 diabetes (1–16% of individuals compared with 0.3–1% in the
general population) (21,22). Symptoms of celiac disease include diarrhea, weight loss
or poor weight gain, abdominal pain, bloating, chronic fatigue, malnutrition due to
malabsorption, and unexplained hypoglycemia or erratic blood glucose levels. Screening
for celiac disease with serum levels of tissue transglutaminase or antiendomysial
antibodies should be considered soon after the diagnosis of diabetes and/or if symptoms
develop. Individuals who test positive should be referred to a gastroenterologist
for possible small-bowel biopsy to confirm the diagnosis, although this is not necessary
in all cases. Symptomatic children with strongly positive antibodies and supportive
genetic or HLA testing may not require a biopsy, but asymptomatic at-risk children
should have a biopsy (23). In symptomatic individuals with type 1 diabetes and confirmed
celiac disease, a gluten-free diet reduces symptoms and decreases rates of hypoglycemia
(24).
Thyroid Disease
About one-quarter of children with type 1 diabetes have thyroid autoantibodies (thyroid
peroxidase antibodies or antithyroglobulin antibodies) at the time of diagnosis (25,26).
The presence of thyroid autoantibodies is predictive of thyroid dysfunction, generally
hypothyroidism and less commonly hyperthyroidism (27). Thyroid dysfunction is more
common in adults with type 1 diabetes, although the exact prevalence is unknown. Women
are more commonly affected than men. Subclinical hypothyroidism, hyperthyroidism,
or coexistent Addison disease (adrenal insufficiency) may also deteriorate metabolic
control with increased risk of symptomatic hypoglycemia (28) and may reduce linear
growth in children (29).
Additional Considerations for Pediatrics
All children require some level of adult supervision in managing their diabetes. Assessments
of pediatric patients should address issues specific to infants/preschoolers, school-aged
children, adolescents, and emerging adults (Table 2). Health care providers should
do a thorough assessment of the developmental needs of the youth (and caregiver),
focusing on physical and emotional development, family issues, and psychosocial needs.
The diabetes treatment plan should be individualized and tailored to the needs of
individual patients and their families. Efforts to achieve target blood glucose and
A1C levels should be balanced with preservation of quality of life and protect against
excessive hypoglycemia.
Height and weight should be measured at each visit and tracked via appropriate height
and weight growth charts. An age-adjusted BMI can be calculated starting at age 2
years. These tools can be found for children and teens at http://apps.nccd.cdc.gov/dnpabmi.
Blood pressure measurements should be determined correctly, using the appropriate
size cuff and with the child seated and relaxed. Hypertension should be confirmed
on at least 3 separate days. Normal blood pressure levels for age, sex, and height
and appropriate methods for determinations are available online at www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf.
Chronic Complications in Children
Retinopathy, nephropathy, and neuropathy rarely have been reported in prepubertal
children and children with diabetes duration of only 1–2 years; however, they may
occur after the onset of puberty or after 5–10 years of diabetes (30). As screening
recommendations are based on recent evidence, these periodically change. Therefore,
we refer the reader to the ADA Standards of Care for the current screening recommendations
for children. It is recommended that those with expertise in diabetes management should
conduct the assessments. For example, ophthalmologic exams should be performed by
those skilled in diabetic retinopathy management and experienced in counseling pediatric
patients and parents on the importance of early prevention/intervention. Another example,
nephrologists with experience with diabetic nephropathy would be aware that intermittent
elevations in urinary albumin excretion are common in pediatric patients, particularly
in association with exercise.
Additional Considerations for Adults
Adults with type 1 diabetes now span a very large age spectrum—from 18 to 100 years
of age and beyond. Unlike the well-characterized developmental stages of children,
the life stages traversed through adulthood are often less well documented and underappreciated.
However, an understanding of each individual’s circumstances is vital. This is true
for aging in general, but particularly true for those with significant comorbidities
due to long-standing type 1 diabetes. Thus, it is important to assess the clinical
needs of the patient, setting specific goals and expectations that may differ significantly
between a healthy 26-year-old and a frail 84-year-old with CVD and retinopathy.
Recommendations
See 2014 ADA Standards of Medical Care for detailed screening information for CVD,
nephropathy, retinopathy, neuropathy, and foot care.
Access to health care should include clinicians with expertise in type 1 diabetes
management, including (but not limited to) an endocrinologist (or other health care
provider with expertise in type 1 diabetes management), a registered dietitian, a
diabetes educator, a mental health professional, an exercise specialist/physiologist,
and specialists required to treat diabetes complications. (E)
Routine follow-up (generally quarterly) should include review of self-monitoring of
blood glucose (SMBG), continuous glucose monitoring (CGM) and pump data (if applicable),
A1C measurement, evidence for acute and/or chronic complications of diabetes (particularly
episodes of DKA and mild and/or severe hypoglycemia), measurement of blood pressure
and weight (and height in children), foot exam, inspection of injection/insertion
sites, and discussion of psychosocial and educational needs (Tables 4 and 5). (E)
Providers should routinely document the patient’s age and disease duration. When clinically
indicated, laboratory measures such as lipids, renal function measurements, and antibodies
for associated autoimmune disease (thyroid or celiac disease) should be documented.
(E)
Parent/guardian involvement in care is required throughout childhood, with a gradual
shift in responsibility of care from the parent/guardian to the youth. (E)
Health care for adults should be focused on the needs of the individual throughout
the various stages of their life, with age-appropriate evaluation and treatment. (E)
Evaluation and treatment of CVD risk should be individualized. (E)
Immunizations should be given as recommended by the Centers for Disease Control and
Prevention (CDC) for children/adults in general and people with diabetes specifically.
(C)
Consider screening for celiac disease by measuring IgA antitissue transglutaminase
or antiendomysial antibodies, with documentation of normal total serum IgA levels,
soon after the diagnosis of diabetes and/or if symptoms develop. Refer the patient
to a gastroenterologist if the test is positive. (E)
Consider screening for thyroid peroxidase and thyroglobulin antibodies soon after
diagnosis. (E)
Screen for thyroid dysfunction by measuring thyroid-stimulating hormone (TSH) concentrations
soon after type 1 diabetes diagnosis (and after stable metabolic control). If normal,
consider rechecking every 1–2 years or more frequently if the patient develops unusual
glycemic variation or symptoms of thyroid dysfunction or thyromegaly. (E)
Assess for the presence of additional autoimmune conditions at diagnosis and if symptoms
develop. (E)
Ongoing nutrition and diabetes self-management education (DSME) and support (DSMS)
are needed to address changes in food preferences, access to food, daily schedules,
activity patterns, and potential barriers to self-care, including the risk of an eating
disorder. (E)
Assess psychosocial status annually and more often as needed; treat and/or refer to
a mental health professional as indicated. (E)
DSME and DSMS
DSME and DSMS are the ongoing processes of facilitating the knowledge, skill, and
ability necessary for diabetes self-care. These processes incorporate the needs, goals,
and life experiences of the person with diabetes. The overall objectives of DSME and
DSMS are to support informed decision making, self-care behaviors, problem solving,
and active collaboration with the health care team to improve clinical outcomes, health
status, and quality of life in a cost-effective manner (31). Because changes in both
treatment and life circumstances occur across the life span, DSME and DSMS must be
a continuous process adapted throughout the life of the person with type 1 diabetes
so that self-management can be sustained.
No matter how sound the medical regimen, it can only be as successful as the ability
of the individual and/or family to implement it. Family involvement remains an important
component of optimal diabetes management throughout childhood and adolescence. Health
care providers who care for children and adolescents must, therefore, be capable of
evaluating the educational, behavioral, emotional, and psychosocial factors that impact
implementation of a treatment plan and must assist the individual and family to overcome
barriers or redefine goals as appropriate (Table 6). Diabetes education should occur
at diagnosis and upon transition to adult diabetes care and should be an ongoing process.
The information needs to be individualized and continually adapted to the patient’s
needs.
Table 6
DSME content based on life stages
Infancy (birth–18 months)
Period of trust versus mistrust
Providing warmth and comfort measures after invasive procedures is important
Feeding and sleeping or nap routines
Vigilance for hypoglycemia
Play age (3–5 years)
Reassurance that body is intact, use of Band-Aids and kisses after procedures
Identification of hypoglycemic signs and symptoms (temper tantrums and nightmares
are common)
Include child in choosing injection and finger-prick sites
Positive reinforcement for cooperation
Begin process for teaching child awareness of hypoglycemia
School age (6–12 years)
Integrate child into educational experience
Determine skill level
Identify self-care skills
Determine roles and responsibilities
Communication with peers and school staff—who and when to tell about diabetes
Adolescence (12–18 years)
Begin transition care planning
Personal meaning of diabetes
Determine roles and responsibilities in care
Social situations and dating
Who or when to tell about diabetes
Driving
Sex and preconception counseling
Alcohol and drugs
College and career planning
Young adults
Personal meaning of diabetes
Roles and responsibilities in care
Social situations and dating
Who or when to tell about diabetes
Genetic risks, conception, and preconception
Travel
Choosing or pursuing a career
Workplace rights
Health or life insurance
Involving friends and significant others in diabetes care
Safety
Creating a support network
Establishing or maintaining independence
Middle-aged adults
Personal meaning of diabetes
Roles and responsibilities in care
Involving spouse or significant other in care
Sexual functioning
Developing a support network
Travel
Pursuing a career
Workplace rights
Health or life insurance
Talking with children or other family members about diabetes
Balancing other responsibilities with diabetes care
Safety
Facing complications
Older adults
Personal meaning of diabetes
Roles and responsibilities in care
Maintaining independence
Obtaining assistance with diabetes care tasks
Involving spouse or significant other in care
Travel
Talking with adult children or other family members about diabetes
Safety
Assessing for declines in ability to perform self-care/activities of daily living
Caring for diabetes along with other chronic illnesses or comorbidities
Obtaining health care when living in multiple locations
Community resources
Care of type 1 diabetes in long-term or other care facilities
Recommendations
Individuals with type 1 diabetes and parents/caregivers (for individuals aged <19
years) should receive culturally sensitive and developmentally appropriate individualized
DSME and DSMS according to national standards for DSME and DSMS when their diabetes
is diagnosed and routinely thereafter. (B)
Additional Considerations for Pediatrics
Education should be provided to appropriate school personnel as a significant portion
of a child’s day is spent in school. (E)
The developing teenager must be educated about the transition to adult health care,
beginning in early to mid-adolescence, with increasing efforts to establish self-reliance
in diabetes care beginning at least 1 year prior to the transition. Even after the
transition to adult care is made, support and reinforcement are recommended. (E)
Additional Considerations for Adults
Adult learning theory can be used to tailor DSME and DSMS to the age, life stage,
culture, literacy/numeracy, knowledge, experience, and cognitive ability of the patient.
(C)
Psychosocial: Assessment and Treatment of Psychosocial Issues
Assessment and appropriate management of psychosocial issues are important throughout
the life span of individuals with type 1 diabetes. In pediatrics, health care providers
should assess the individual child and the child’s family for their ability to function
and behave appropriately regarding safe and responsible diabetes care. For adults,
the individual is the focus of care. However, family involvement should be strongly
encouraged when appropriate.
Depression screening and discussion about psychosocial issues are important components
of the diabetes visit. Special attention should be paid to diabetes-related distress,
fear of hypoglycemia (and hyperglycemia), eating disorders, insulin omission, subclinical
depression, and clinical depression. These factors are significantly associated with
poor diabetes self-management, a lower quality of life, and higher rates of diabetes
complications. As individuals age, health care providers should evaluate issues related
to self-care capacity, mobility, and autonomy. Such factors are to be promptly addressed,
as they make the management of type 1 diabetes ever more problematic.
Recommendations
Make age-appropriate screenings for psychosocial issues a component of most diabetes
visits. Any concerns should be pursued through treatment that may include referral
to a mental health specialist. (E)
Additional Considerations for Pediatrics
Ensure that there is developmentally appropriate parent/family involvement in the
management of the child’s/adolescent’s diabetes care tasks, avoiding a premature transfer
of sole responsibility for diabetes management to the developing child/teenager. (B)
Directly ask about diabetes-related family conflict and stress and negotiate an acceptable
resolution with the child/adolescent and parent(s). However, if family conflict is
extremely entrenched and cannot be resolved by the diabetes team, referral should
be made to a mental health specialist who is knowledgeable about type 1 diabetes in
youth and family functioning. (C)
Additional Considerations for Adults
Ongoing evaluation of patients’ general and diabetes-related quality of life, emotional
well-being, distress, depression, and resources is warranted, preferably by a team
that includes a mental health specialist if such resources are available. (C)
Health care providers should promptly address issues related to self-care capacity,
mobility, and autonomy. (E)
Nutrition Therapy
Nutrition therapy is an important component of the treatment plan for all individuals
with type 1 diabetes. Each patient should have an individualized food plan based on
food preferences, schedule, and physical activity. Nutrition therapy aims to ensure
that the patient and family understand the impact food has on blood glucose, how food
interacts with exercise and insulin to prevent hypo- and hyperglycemia and to achieve
glucose goals, and how to implement the food plan in a variety of situations. The
food plan takes into consideration the patient’s numeracy, literacy, engagement, and
ability to adjust insulin.
General diabetes nutrition principles, as defined in the ADA Standards of Care, apply
to people with type 1 diabetes, particularly in reference to normal growth and development
in youth and the maintenance of a healthy body weight at all ages. Specifically, with
regards to individuals with type 1 diabetes, topics such as carbohydrate counting
and meal composition should be addressed. For selected individuals who have mastered
carbohydrate counting, education on the impact of protein and fat on glycemic excursions
should be incorporated into diabetes management (32). Those who are overweight or
obese may benefit from weight reduction counseling.
Recommendations
Individualized medical nutrition therapy is recommended for all people with type 1
diabetes as an effective component of the overall treatment plan. (A)
Monitoring carbohydrate intake, whether by carbohydrate counting or experience-based
estimation, remains a key strategy in achieving glycemic control. (B)
If adults with type 1 diabetes choose to drink alcohol, they should be advised to
do so in moderation (one drink per day or less for adult women and two drinks per
day or less for adult men). Discussion with a health care provider is advised to explore
potential interactions with medications. Adults should be advised that alcohol can
lower blood glucose levels and that driving after drinking alcohol is contraindicated.
(E)
Physical Activity and Exercise
Exercise has many positive health and psychological benefits including physical fitness,
weight management, and enhanced insulin sensitivity. It also provides opportunities
for social interactions and builds self-esteem. However, exercise creates challenges
for people with type 1 diabetes due to the increased risk for both hypoglycemia and
hyperglycemia. During exercise, multiple hormones (insulin, glucagon, catecholamines,
growth hormone, and cortisol) control fuel metabolism and create a balance between
glucose uptake by exercising muscles and hepatic glucose production (33,34). The equilibrium
between insulin secretion and the counterregulatory hormones varies according to the
exercise type, intensity, and duration (35).
Hyperglycemia results from counterregulatory hormone excess with insufficient insulin,
leading to excessive hepatic glucose production and limiting increased glucose uptake
into skeletal muscle. Hyperglycemia can occur before, during, and after various types
of exercise. If the patient feels well, with negative or minimal urine and/or blood
ketones, and there is a clear reason for the elevated blood glucose level, such as
underdosing insulin at the preceding meal, it is not necessary to postpone exercise
based solely on hyperglycemia. However, when people with type 1 diabetes are deprived
of insulin for 12–48 h and are ketotic, exercise can worsen hyperglycemia and ketosis.
Therefore, vigorous activity should be avoided in the presence of severe hyperglycemia
and ketosis, especially with known insulin omission.
Physical activity increases hypoglycemia risk during and immediately following exercise,
and, again, about 7–11 h postexercise. This delayed susceptibility to hypoglycemia
is referred to as the “lag effect” of exercise (36,37) and is caused by muscles replenishing
glycogen stores postexercise. Hypoglycemia and fear of hypoglycemia can limit participation
in exercise.
Strategies should be developed to prevent and treat hypoglycemia readily. Individualization
is necessary, but clinical experience suggests that it is safest for most patients
to have a blood glucose level of 100 mg/dL (5.6 mmol/L) or higher prior to starting
exercise. This may be achieved by reducing the prandial insulin dose for the meal/snack
preceding exercise and/or increasing food intake. Some patients can avoid hypoglycemia
by reducing insulin (such as by lowering pump basal rates) (38) or by consuming additional
carbohydrates during prolonged physical activity. One study in children on pumps suggested
that a reduction in overnight basal insulin the night following exercise may reduce
the risk of delayed exercise-induced hypoglycemia (39). Frequent SMBG and/or CGM use
are key to exercising safely, as is ready access to carbohydrates.
Basic recommendations for physical activity are the same as those for all children
and adults, independent of the diagnosis of diabetes: children should be encouraged
to engage in at least 60 min of physical activity daily, and adults should be advised
to perform at least 150 min/week of moderate-intensity aerobic physical activity (50–70%
of maximum heart rate) or a lesser amount (60–75 min/week) of vigorous-intensity activity
(40,41). Exercise should also include resistance and flexibility training.
Individuals, particularly adults, should be assessed for cardiovascular risk and the
presence of complications that might limit exercise as discussed more fully in the
ADA Standards of Medical Care in Diabetes (42).
Recommendations
Exercise should be a standard recommendation as it is for individuals without diabetes;
however, recommendations may need modifications due to the presence of macro- and
microvascular diabetes complications. (E)
Patients of all ages (or caregivers of children) should be educated about the prevention
and management of hypoglycemia that may occur during or after exercise. (E)
Patients should be advised about safe preexercise blood glucose levels (typically
100 mg/dL or higher depending on the individual and type of physical activity). (E)
Reducing the prandial insulin dose for the meal/snack preceding exercise and/or increasing
food intake can be used to help raise the preexercise blood glucose level and reduce
hypoglycemia. (E)
A reduction in overnight basal insulin the night following exercise may reduce the
risk for delayed exercise-induced hypoglycemia. (C)
SMBG should be performed as frequently as needed (before, during, and after exercise)
in order to prevent, detect, and treat hypoglycemia and hyperglycemia. (E)
Source(s) of simple carbohydrate should be readily available before, during, and after
exercise to prevent and treat hypoglycemia. (E)
Treatment Targets
General Considerations
Hyperglycemia defines diabetes and is directly related to the incidence of complications.
Therefore, glycemic control is fundamental to diabetes management. The Diabetes Control
and Complications Trial (DCCT) (43) was a prospective randomized controlled study
comparing intensive versus standard glycemic control in patients diagnosed with type
1 diabetes relatively recently. The DCCT demonstrated that achieving an A1C of <7%
reduced the incidence of microvascular complications of type 1 diabetes compared with
standard control, which achieved an A1C of ∼9% during the period of the randomized
trial. The Epidemiology of Diabetes Interventions and Complications (EDIC) study (44,45)
was a follow-up of the DCCT cohorts. The EDIC study remarkably demonstrated persistent
microvascular and cardiovascular benefits in subjects who had previously received
intensive treatment, even though their glycemic control had deteriorated over time.
While A1C and blood glucose targets are needed, the ADA emphasizes that glycemic targets
should be individualized with the goal of achieving the best possible control while
minimizing the risk of severe hyperglycemia and hypoglycemia (Table 7). Goals should
be individualized based on duration of diabetes, age/life expectancy, comorbid conditions,
known CVD or advanced microvascular complications, hypoglycemia unawareness, and individual
patient considerations. More or less stringent glycemic goals may be appropriate for
individual patients. Postprandial glucose may be targeted if A1C goals are not met
despite reaching preprandial glucose goals.
Table 7
Summary of A1C recommendations for nonpregnant people with diabetes*
Youth (<18 years)
<7.5%
Adults
<7.0%
Older adults
Healthy†
<7.5%
Complex/intermediate
<8.0%
Very complex/poor health
<8.5%
*
Targets must be individualized based on a patient's circumstances.
†
No comorbidities, long life expectancy.
Recommendation
Lifestyle, psychosocial, and medical circumstances should be considered when recommending
glycemic goals for all age-groups. (E)
Glycemic Control Goals in Pediatrics
As the DCCT only included pediatric patients aged ≥13 years (195 adolescents aged
13–17 years at entry), treatment guidelines for pediatric patients have been based
nearly exclusively on professional, expert advice. Furthermore, despite the overall
A1C goal of <7% for adults with type 1 diabetes, pediatric patients, aged 13–19 years,
had an A1C target of <7.5%. This slightly higher A1C target for adolescents with type
1 diabetes was based on expert recommendations and the clinical reality that optimizing
glycemic control in adolescent patients with type 1 diabetes is especially challenging,
given the physiological and behavioral challenges that confront this age-group.
The ADA’s blood glucose and A1C goals traditionally have been developmentally or age
based in the pediatric population, but it is now time to alter the traditional goals
based on recent data. The traditional recommendations are an A1C goal of <8.5% for
youth under the age of 6 years, <8% for those 6–12 years old, and <7.5% for those
13–19 years old. Lower blood glucose levels and lower A1C targets should be pursued
as long as patients can avoid severe, recurrent hypoglycemia. Thus, the overall recommendation
has included the goal to achieve as close to normal blood glucose and A1C levels as
is possible without the occurrence of severe, recurrent hypoglycemia.
Historically, the ADA recommended higher A1C targets for young children. This recommendation
arose from a combination of two lines of unsubstantiated evidence. First, an older
body of literature, reflecting therapy in the premodern era, devoid of insulin analogs,
easy-to-use blood glucose monitors, “smart pumps,” and CGM devices, indicated that
severe recurrent hypoglycemia with seizure and/or coma in young children was associated
with neurocognitive compromise (46). The second line of evidence arose from literature
that questioned what, if any, impact blood glucose and A1C levels prior to puberty
have on the risk for the development of future long-term complications of diabetes
(47,48). With the combination of these two independent lines of reports, it is not
surprising that earlier recommendations regarding glycemic targets focused on the
avoidance of severe hypoglycemia in order to reduce risk of neurocognitive dysfunction,
especially in young children and even school-aged children.
Currently, treatment strategies for children recommend physiological insulin replacement
with modern strategies and treatment tools. More recent investigation and active ongoing
research have dispelled concerns regarding hypoglycemia and neurocognitive dysfunction
(49,50).
Studies assessing neurocognitive function have failed to identify adverse effects
of a past history of hypoglycemia in the young child; however, as always, further
research needs to be conducted.
There are also questions regarding the premise that the years prior to puberty do
not impact the future risk of complications (51). Many investigators and clinicians
believe in the importance of controlling blood glucose and A1C levels prior to puberty
to reduce risk for both micro- and macrovascular complications. Additionally, there
is burgeoning evidence that elevated blood glucose levels and glycemic variability
in the very young child with diabetes may produce adverse outcomes in the short term
on neurocognitive function and the central nervous system (52,53). These recent articles
suggest that hyperglycemia and glycemic variability are associated with changes in
the central nervous system white matter, as observed in MRI scans.
Taking into account the combination of spotty past evidence related to the adverse
effects of hypoglycemia on the developing brain and increasing evidence from more
recent investigations focused on the potential risks of hyperglycemia and glucose
variability on the central nervous system, the ADA has decided to alter the recommendations
for glycemic targets in pediatric patients with type 1 diabetes and harmonize with
other organizations. The International Society for Pediatric and Adolescent Diabetes
(ISPAD) uses a single A1C goal of <7.5% across all pediatric age-groups. This recommendation
is based on clinical studies and expert opinion, as rigorous evidence does not currently
exist. Specifically, the recommendation is derived from a combination of clinical
experience and intensive management strategies that provide opportunities to achieve
as near-normal glycemic control as possible without the occurrence of severe hypoglycemia.
In light of the above evidence, the ADA will harmonize its glycemic goals with those
of ISPAD (as well as the Pediatric Endocrine Society and the International Diabetes
Federation) by using a single A1C goal of <7.5% across all pediatric age-groups.
However, as mentioned previously, it must be emphasized that the ADA strongly believes
that blood glucose and A1C targets should be individualized with the goal of achieving
the best possible control while minimizing the risk of severe hyperglycemia and hypoglycemia
and maintaining normal growth and development.
Recommendation
An A1C goal of <7.5% is recommended across all pediatric age-groups. (E)
Glycemic Control Goals in Adults
Similar to in children, the care of older adults with diabetes is complicated by their
clinical and functional heterogeneity. Unlike the large older adult population with
type 2 diabetes, which includes patients with both long-standing and new-onset diabetes,
most older adults with type 1 diabetes have long-standing disease. Even so, there
is a wide spectrum of health across older individuals. They may have advanced complications,
or they may have lived with diabetes for many years without the development of complications.
Some older patients have multiple comorbid conditions and/or impairments of physical
or cognitive functioning, while others have little comorbidity and high functional
status. Life expectancy is highly variable and is defined by comorbidity and functional
status more than it is by age.
Health care providers caring for older adults with diabetes must take this heterogeneity
into consideration when setting and prioritizing treatment goals. The benefits of
interventions such as stringent glycemic control may not apply to those with advanced
complications of diabetes or to those with a life expectancy of less than the anticipated
time frame of benefit. Conversely, the risks of interventions such as tight glycemic
control (hypoglycemia, treatment burden) may be greater in older patients. Although
individualization is critical, in general, older patients with long life expectancy
and little comorbidity should have treatment targets similar to those of middle-aged
or younger adults. In more frail patients, treatment targets might reasonably be relaxed,
while symptomatic hyperglycemia or the risk of DKA should still be avoided (54).
Recommendations
Lowering A1C to below or around 7% has been shown to reduce microvascular complications
of diabetes, and, if achieved soon after the diagnosis of diabetes, is associated
with long-term reduction in macrovascular disease. Therefore, a reasonable A1C goal
for many nonpregnant adults with type 1 diabetes is <7%. (B)
Providers might reasonably suggest more stringent A1C goals (such as <6.5%) for select
individual patients, if this can be achieved without significant hypoglycemia or other
adverse effects of treatment. Appropriate patients might include those with a short
duration of diabetes, a long life expectancy, hypoglycemia awareness, and no significant
CVD. (C)
Less stringent A1C goals (such as <8.5%) may be appropriate for patients with a history
of severe hypoglycemia, hypoglycemia unawareness, limited life expectancy, advanced
microvascular/macrovascular complications, or extensive comorbid conditions. (B)
Glycemic control for those of any age with type 1 diabetes should be assessed based
on frequent SMBG levels (and CGM data, if available) in addition to A1C in order to
direct changes in therapy. (B)
Monitoring
SMBG
The DCCT demonstrated the benefits of intensive glycemic control on diabetes complications
with SMBG as part of a multifactorial intervention, suggesting that SMBG is a crucial
component of effective therapy. SMBG allows patients to evaluate their individual
response to therapy and assess whether glycemic targets are being achieved. SMBG results
are useful in preventing hypoglycemia, adjusting medications (particularly prandial
insulin doses), and understanding the impact of appropriate nutrition therapy and
physical activity. More frequent SMBG is correlated to lower A1C levels (55,56).
SMBG frequency and timing should be dictated by the patient’s specific needs and goals.
When prescribing SMBG, providers must ensure that patients receive ongoing instruction
and regular evaluation of their SMBG technique and their ability to use SMBG data
to adjust therapy (insulin and/or food). Furthermore, SMBG results should be downloaded
and reviewed at each visit.
SMBG is especially important for patients with type 1 diabetes to monitor for and
prevent asymptomatic hypoglycemia and hyperglycemia. Type 1 diabetic patients should
perform SMBG prior to, and sometimes after, meals and snacks, at bedtime, before and
after exercise, when they suspect low blood glucose, after treating low blood glucose
until they are normoglycemic, and prior to critical tasks such as driving. For many
patients, this will require testing 6–10 times daily, although individual needs may
vary. For example, sick children may require up to 10 SMBG tests per day or more.
A study of children and adolescents with type 1 diabetes showed that, after adjustment
for multiple confounders, increased SMBG frequency was significantly associated with
lower A1C. In the range of 0–5 tests per day, A1C decreased by 0.46% per additional
test per day. Increased testing was associated with significantly less DKA and (probably
due to reverse causality) significantly more hypoglycemia (55,56).
SMBG accuracy is dependent on both the instrument and the user (57), so it is important
to evaluate each patient’s monitoring technique, both initially and at regular intervals
thereafter. Optimal use of SMBG requires a proper review and interpretation of the
data by both the patient and the provider.
CGM
Real-time CGM through the measurement of interstitial glucose (which correlates well
with plasma glucose) is available. These sensors require calibration with SMBG, and
CGM users still require SMBG for making acute treatment decisions. CGM devices have
alarms for hypo- and hyperglycemic excursions that include absolute level and rate-of-change
alerts. A 26-week randomized trial of 322 type 1 diabetic patients showed that adults
aged ≥25 years using intensive insulin therapy and CGM experienced a 0.5% reduction
in A1C (from ∼7.6% to 7.1%) compared with usual intensive insulin therapy with SMBG
(58). Participants aged <25 years (children, teenagers, and young adults) randomized
to sensor use did not achieve a significant A1C reduction. However, these younger
patients did not use CGM consistently. The greatest predictor of A1C lowering for
all age-groups was frequency of sensor use, which was lowest in 15- to 24-year-old
subjects. There was no significant difference in hypoglycemia in any age-group. In
a smaller randomized controlled trial of 129 adults and children with baseline A1C
<7.0%, outcomes combining A1C and hypoglycemia favored the group using CGM, suggesting
that CGM is beneficial for pediatric patients and adults with type 1 diabetes who
have already achieved excellent control (58).
Overall, meta-analyses suggest that, compared with SMBG, CGM use is associated with
A1C lowering by ∼0.26% (59) without an increase in hypoglycemia, although existing
studies have small sample sizes and are of relatively short duration. The technology
may be particularly useful in those with hypoglycemia unawareness and/or frequent
hypoglycemic episodes, although studies have not consistently shown significant reductions
in the occurrence of severe hypoglycemia. A CGM device equipped with an automatic
low threshold suspend feature was approved by the U.S. Food and Drug Administration
(FDA) in 2013. The Automation to Simulate Pancreatic Insulin Response (ASPIRE) trial
of 247 patients showed that sensor-augmented insulin pump therapy with a low glucose
suspend feature significantly reduced nocturnal hypoglycemia without increasing A1C
levels for those >16 years of age (60). These devices may offer the opportunity to
reduce severe hypoglycemia for those with a history of nocturnal hypoglycemia, although
more clinical trials are needed.
Recommendations
Patients with type 1 diabetes should perform SMBG prior to meals and snacks, at a
minimum, and at other times, including postprandially to assess insulin-to-carbohydrate
ratios; at bedtime; midsleep; prior to, during, and/or after exercise; when they suspect
low blood glucose; after treating low blood glucose until they have restored normoglycemia;
when correcting a high blood glucose level; prior to critical tasks such as driving;
and at more frequent intervals during illness or stress. (B)
Individuals with type 1 diabetes need to have unimpeded access to glucose test strips
for blood glucose testing. Regardless of age, individuals may require 10 or more strips
daily to monitor for hypoglycemia, assess insulin needs prior to eating, and determine
if their blood glucose level is safe enough for overnight sleeping. (B)
CGM is a useful tool to reduce A1C levels in adults without increasing hypoglycemia
and can reduce glycemic excursions in children. Glycemic improvements are correlated
with frequency of CGM use across all ages. (A)
Additional Considerations for Pediatrics
Children should have additional blood glucose checks if the parent/caregiver is concerned
that the child’s behavior may be due to low/high blood glucose levels. (E)
School employees and caregivers should be knowledgeable about SMBG and equipped with
all necessary supplies. (E)
Capable children should be permitted to self-manage their diabetes at school. (E)
A1C Testing
A1C reflects average glycemia over 2–3 months (57) and strongly predicts diabetes
complications (43,61). Thus, A1C testing should be performed routinely in all patients
with diabetes at initial assessment and as part of continuing care. A1C is a convenient
method to track diabetes control; however, there are disadvantages. Glycation rates,
and thus A1C levels, may vary with patients’ race/ethnicity. However, this is controversial.
Additionally, anemias, hemoglobinopathies, and situations of abnormal red cell turnover
affect A1C (42).
A1C measurements approximately every 3 months determine whether a patient’s glycemic
targets have been reached and maintained. For any individual patient, the frequency
of A1C testing should be dependent on the clinical situation, the treatment regimen
used, and the clinician’s judgment. Unstable or highly intensively managed patients
(e.g., pregnant type 1 diabetic women) may require more frequent testing than every
3 months (62). In patients with hemoglobinopathies that interfere with the A1C assay
or with hemolytic anemia or other conditions that shorten the red blood cell life
span, the A1C may not accurately reflect glycemic control or correlate well with SMBG
testing results. In such conditions, fructosamine may be considered as a substitute
measure of long-term (average over 2 weeks) glycemic control.
Recommendations
Perform the A1C test quarterly in most patients with type 1 diabetes and more frequently
as clinically indicated (i.e., pregnancy). (A)
Point-of-care A1C testing, using a DCCT standardized assay, may provide an opportunity
for more timely treatment changes. (E)
Insulin Therapy
The DCCT clearly showed that intensive insulin therapy, defined as three or more injections
per day of insulin or continuous subcutaneous insulin infusion (CSII) (or insulin
pump therapy), was a key part of improved glycemia and better outcomes (43,63). The
study was carried out with short- and intermediate-acting human insulins. Despite
better microvascular outcomes, intensive insulin therapy was associated with a high
rate of severe hypoglycemia (62 episodes per 100 patient-years of therapy). Since
the completion of the DCCT, a number of rapid-acting and long-acting insulin analogs
have been developed. These analogs are associated with less hypoglycemia than human
insulin while offering the same amount of A1C lowering in people with type 1 diabetes
(64,65).
The Sensor-Augmented Pump Therapy for A1C Reduction (STAR 3) study was a large (n
= 485) randomized clinical trial comparing insulin pump therapy and CGM with insulin
injections in youth and adults with type 1 diabetes. The two study groups started
with the same baseline A1C of 8.3%. After 1 year, the group using insulin pump therapy
and CGM had lower A1C levels (7.5% vs. 8.1%, P < 0.001) without significant nocturnal
hypoglycemia compared with the insulin injection cohort (66). Recently, a large randomized
trial in patients with type 1 diabetes and nocturnal hypoglycemia reported that the
use of sensor-augmented insulin pump therapy with the threshold-suspend feature reduced
nocturnal hypoglycemia without increasing glycated hemoglobin values (60). In general,
intensive management using pump therapy/CGM should be strongly encouraged, with active
patient/family participation enhancing successful outcomes (67–69).
Recommendations
Most individuals with type 1 diabetes should be treated with multiple daily insulin
injections (three or more injections per day of prandial insulin and one to two injections
of basal insulin) or CSII. (A)
Most individuals with type 1 diabetes should be educated in how to match prandial
insulin dose to carbohydrate intake, premeal blood glucose, and anticipated activity.
(E)
Most individuals with type 1 diabetes should use insulin analogs to reduce hypoglycemia
risk. (A)
All individuals with type 1 diabetes should be taught how to manage blood glucose
levels under varying circumstances, such as when ill or receiving glucocorticoids
or for those on pumps, when pump problems arise. (E)
Child caregivers and school personnel should be taught how to administer insulin based
on provider orders when a child cannot self-manage and is out of the care and control
of his or her parent/guardian. (E)
Interdiction
Therapy trials to prevent type 1 diabetes development (prevention), to preserve remaining
β-cells (preservation), and to replace β-cells (transplantation) are ongoing. Although
means are available to screen and predict family members at risk for developing type
1 diabetes, efforts to delay or prevent disease onset have been largely disappointing.
A variety of different immunomodulatory and immune-suppressive agents have been evaluated
in patients with recent-onset type 1 diabetes, and the effects have been modest at
best: for the subset of drugs that appear to have an effect, not all patients respond;
for those who do, the effects are generally transient. Many of the agents tested to
date are FDA approved for other indications, but given the observations to date and
potential toxicities, the recommendation is that patients should only receive these
drugs after being enrolled in clinical research protocols with appropriate follow-up.
Long-term safety and efficacy data are scarce, especially in children. Investigators
continue to evaluate promising new agents and combinations of drugs or cell-based
therapies in an effort to safely and effectively modulate the autoimmune response
(70).
β-Cell Replacement Therapy
β-Cell replacement may be achieved through pancreas or islet transplantation in select
candidates. Pancreas transplants are now accepted as a proven therapy, while islet
transplants, though significantly improving, are still mostly done on an experimental
basis.
Pancreas Transplants
Pancreas transplants are most often performed in combination with kidney transplantation,
either as a simultaneous pancreas-kidney (SPK) transplant or as a pancreas-after-kidney
(PAK) transplant (71). SPK and PAK transplants may be considered for individuals with
late-stage kidney disease because the transplants can normalize glucose levels, which
will prevent hypoglycemia and provide some protection for the transplanted kidney
(72), and provide other benefits, including an improvement in quality of life (71).
These recipients will already require immunosuppression for their renal transplants,
which means the major additional risk is the operative procedure. SPK transplants
function for an average of 9 years, compared with 6 years for PAK transplants (71).
There has been debate about pancreas transplant alone (PTA) in the absence of an indication
for kidney transplantation because of the risks of mortality, morbidity, and immunosuppression.
Outcomes have gradually improved (73), such that the procedure can be cautiously considered
for individuals without renal failure who have unstable glucose control and hypoglycemia
unawareness. Because of the risks of pancreas transplantation compared with traditional
methods for controlling blood glucose levels, all available efforts to use exogenous
insulin combined with technology, education, and glucose follow-up should be exhausted
before PTA is performed. The durability of function averages 6 years, which is much
better than islet transplantation but about the same as PAK and not as good as SPK
(73).
Islet Transplantation
A major appeal of islet transplantation is that it does not require major surgery.
Moreover, outcomes have improved over the past decade such that normoglycemia without
insulin is now maintained for an average of 3 years in specialized protocols (74).
Even when insulin treatment is reinstituted, residual insulin secretion can help recipients
maintain good control with less hypoglycemia and a less complicated regimen for several
more years.
At the present time, few islet transplants are being performed and most are experimental.
However, they can be considered as a treatment option for those who are poor candidates
for whole-organ transplants. Importantly, their current success has established a
proof of principle for cellular transplantation. Great progress is being made in finding
an abundant source of healthy insulin-producing cells and in developing better ways
to protect transplanted cells from immune destruction (75,76). Potential solutions
for the shortage of islets include embryonic stem cells, induced pluripotent stem
cells, xenogeneic tissue, and various other potential sources—all the focus of ongoing
research efforts. Another possible way to replenish the β-cell deficiency of diabetes
is through regeneration of the endocrine pancreas; this too is being worked on intensively.
Recommendations
Consider solid organ pancreas transplantation simultaneously with kidney transplantation
in patients with type 1 diabetes who have an indication for kidney transplantation
and are poorly controlled with large glycemic excursions. (B)
Consider solid organ pancreas transplantation after kidney transplantation in adult
patients with type 1 diabetes who have already received a kidney transplant. (C)
Judiciously consider solid organ pancreas transplantation alone in adults with type
1 diabetes, unstable glucose control, hypoglycemia unawareness, and an increased risk
of diabetes-related mortality, who have attempted all of the more traditional approaches
to glycemic control and have remained unsuccessful, yet are judged responsible enough
to manage the antirejection medication regimen, risks, and follow-up required with
an organ transplant. (C)
Consider referral to research centers for protocolized islet cell transplantation
in patients with type 1 diabetes and debilitating complications of diabetes who are
interested in research possibilities and fit the criteria for the research protocol.
(E)
Adjunctive Therapies
Pramlintide
Pramlintide, an amylin analog, is an agent that delays gastric emptying, blunts pancreatic
secretion of glucagon, and enhances satiety. It is an FDA-approved therapy for use
in type 1 diabetic patients and has been shown to reduce A1C, induce weight loss,
and lower insulin dose. However, it is only indicated for adults. Two 52-week trials
of pramlintide (n = 1,131; age >18 years) showed A1C reductions of ∼0.3–0.4% (77,78).
In both studies, a greater proportion of participants achieved an A1C target of <7%
with the therapy than without the therapy. There are a few small, short-term studies
of pramlintide use in children with type 1 diabetes, with outcomes similar to those
in the adult studies. Clearly, larger, long-term studies are needed in pediatrics.
Incretin-Based Therapies
Injectable glucagon-like peptide-1 (GLP-1) agonists and oral dipeptidyl peptidase-4
(DPP-4) inhibitors are increasingly being studied in the type 1 diabetic population,
but are not approved by the FDA for this indication. GLP-1 agonists delay gastric
emptying, suppress the postprandial rise in glucagon secretion, and may increase satiety.
Preliminary studies indicate that these agents may also facilitate weight loss. Further
long-term clinical trials in type 1 diabetic patients are needed.
Sodium-Glucose Cotransporter 2 Inhibitors
Sodium-glucose cotransporter 2 (SGLT2) inhibitors work by inhibiting glucose reabsorption
in the kidney and are also being tested in individuals with type 1 diabetes. These
agents provide insulin-independent glucose lowering by blocking glucose reabsorption
in the proximal renal tubule, leading to weight loss and A1C reduction in individuals
with type 2 diabetes. However, insufficient data exist to recommend clinical use of
these agents in type 1 diabetes at this time.
Metformin
Metformin is a biguanide that decreases hepatic gluconeogenesis and is used as first-line
therapy in type 2 diabetes. It has been shown to have some benefit in reducing insulin
doses and weight in small studies in patients with type 1 diabetes (79) and is now
being evaluated more fully for use in patients with type 1 diabetes. Two randomized
controlled trials are currently under way evaluating metformin in type 1 diabetic
patients. The first study is in adults and is using carotid intima-medial thickness
as an outcome measure (ClinicalTrials.gov identifier: NCT01483560). The second study
is focusing on overweight or obese youths between the ages of 12 and 19 years who
require ≥0.85 units/kg/day of insulin (ClinicalTrials.gov identifier: NCT01808690).
Results are currently pending.
Recommendations
Pramlintide may be considered for use as adjunctive therapy to prandial insulin in
adults with type 1 diabetes failing to achieve glycemic goals. (B)
Evidence suggests that adding metformin to insulin therapy may reduce insulin requirements
and improve metabolic control in overweight/obese patients and poorly controlled adolescents
with type 1 diabetes, but evidence from larger longitudinal studies is required. (C)
Current type 2 diabetes medications (GLP-1 agonists, DPP-4 inhibitors, and SGLT2 inhibitors)
may be potential therapies for type 1 diabetic patients, but require large clinical
trials before use in type 1 diabetic patients. (E)
Hypoglycemia
Hypoglycemia risk is the limiting step in the treatment of type 1 diabetes at any
age. Because current methods of blood glucose detection and insulin replacement are
imperfect (though improved from prior eras), hypoglycemia risk is invariably present.
Patient education (80), frequent SMBG, and CGM can help detect hypoglycemia and allow
for adjustments in insulin dosing and carbohydrate intake. Severe hypoglycemia rates
increase with antecedent episodes of hypoglycemia, age, and duration of diabetes;
thus, this is an issue that must be reassessed frequently (81). Hypoglycemia unawareness
is related to a reduced sympathoadrenal response to hypoglycemia; it can occur in
the setting of recurrent hypoglycemia or autonomic failure and can be reversed by
scrupulous avoidance of hypoglycemia. Patients should be screened to determine the
threshold at which hypoglycemia symptoms occur; if the threshold is suggestive of
hypoglycemia unawareness, the treatment goals and regimen should be revisited and
counseling regarding appropriate self-monitoring before critical tasks should be reinforced
(82).
Oral carbohydrate is the treatment of choice for self-treatment or for the treatment
of hypoglycemic adults and children who are alert and able to eat. Glucagon is used
for severe hypoglycemia. In children, small studies have led to the concept of using
age-based mini-dose glucagon if the child is alert but not able to eat (83).
Recommendations
Individuals with type 1 diabetes, or their caregivers, should be asked about symptomatic
and asymptomatic hypoglycemia at each encounter. (E)
Glucose (15–20 g) is the preferred treatment for the conscious individual with hypoglycemia,
although any form of carbohydrate may be used. If the SMBG result 15 min after treatment
shows continued hypoglycemia, the treatment should be repeated. Once blood glucose
concentration returns to normal, the individual should consume a meal or snack to
prevent recurrence of hypoglycemia. (E)
Glucagon should be prescribed for all individuals with type 1 diabetes. Caregivers
or family members of these individuals should be instructed in its administration.
(E)
Hypoglycemia unawareness or one or more episodes of severe hypoglycemia should trigger
reevaluation of the treatment regimen. (E)
Insulin-treated patients with hypoglycemia unawareness or an episode of severe hypoglycemia
should be advised to raise their glycemic targets to strictly avoid further hypoglycemia
for at least several weeks to partially reverse hypoglycemia unawareness and reduce
the risk of future episodes. (B)
DKA
DKA (see ref. 70 for definition) is an acute complication of diabetes that can be
associated with new-onset type 1 diabetes, insulin omission, and increased levels
of counterregulatory hormones/cytokines associated with stress, such as an infection.
Mild cases can be safely and effectively treated in an acute care setting with appropriate
resources and may not require hospitalization. Education must be provided to individuals
with type 1 diabetes in order to help prevent DKA, which can have serious sequelae,
particularly in children under 5 years of age. Although DKA and hyperglycemic hyperosmolar
state (HHS) may overlap, especially when dehydration is severe, DKA must be distinguished
from HHS (serum glucose >600 mg/dL, serum osmolality >330 mOsm/kg, and no significant
ketosis and acidosis) because patients with HHS typically are severely dehydrated
and require more aggressive fluid management. There are multiple guidelines available
for the management of DKA (84).
Recommendations
Individuals and caregivers of individuals with type 1 diabetes should be educated
and reminded annually how to prevent DKA, including a review of sick-day rules and
the critical importance of always administering insulin and monitoring both glucose
and ketone levels. (B)
Insulin omission is the major cause of DKA; therefore, individuals with type 1 diabetes
must have access to an uninterrupted supply of insulin. (E)
Patients with type 1 diabetes and their families should have around-the-clock access
to medical advice and support to assist with sick-day management. (C)
Standard protocols for DKA treatment should be available in emergency departments
and hospitals. (E)
CVD Screening and Treatment
Much of the existing data on the risk of CVD in individuals with diabetes is based
on people with type 2 diabetes who often have additional CVD risk factors, such as
metabolic syndrome, hypertension, and dyslipidemia. How much is applicable to people
with type 1 diabetes is unknown. However, people with type 1 diabetes are at increased
risk for CVD, particularly those with additional risk factors.
In type 1 diabetes, standard risk factors apply, such as hyperlipidemia, hypertension,
age, family history, smoking, weight, and presence of albuminuria. As such, these
should be considered when determining the need for evaluation and treatment for CVD.
However, even in the absence of classic risk factors, there may be high CVD risk.
An adult with childhood-onset type 1 diabetes of 20-year duration has a substantially
increased risk of coronary artery disease of 1% per year (83), thus meriting high-intensity
statin therapy according to the new joint American College of Cardiology/American
Heart Association guidelines (≥7.5% 10-year risk) (85). In some cases, measurement
of coronary artery calcification may be a helpful method for determining CVD risk
(86). Here, as with all management issues for people with type 1 diabetes, providers
need to individualize assessment and treatment options.
With regard to treatment, statin therapy is the preferred treatment for lipid lowering/CVD
risk reduction (85). The Heart Protection Study (HPS) did include type 1 diabetic
participants who appeared to experience the same degree of benefit from statins as
others in the study, though the finding was not statistically significant due to low
numbers (87). Unfortunately, there are no blood pressure intervention trials with
CVD end points in type 1 diabetes and only one LDL cholesterol–lowering trial (85).
Statin and aspirin therapy (if not contraindicated) should be considered and used
as is individually indicated.
Recommendations
Therapy for those under age 40 years with less than a 20-year diabetes duration (or
over age 75 years) should be considered on an individual basis, though, depending
on overall risk, an LDL cholesterol <100 mg/dL has been suggested as an appropriate
goal with statin intervention for those with LDL cholesterol levels of 130–160 mg/dL.
(E)
Individuals with type 1 diabetes aged 40–75 years may benefit from moderate-to-intensive
statin therapy with consideration of diabetes duration and CVD risk factors. If 10-year
risk is estimated to be ≥7.5%, then intensive statin therapy should be considered.
(B)
Specific Settings and Populations
Pregnancy
Preconception Counseling and Care
To minimize risks associated with pregnancy and type 1 diabetes, preconception counseling
and care are critical. Preconception care with tight glycemic control improves outcomes
including lower cesarean rates (88), decreased perinatal mortality (89–91), and decreased
congenital malformations (89–97). Although there is some evidence that childbearing
may be reduced (98–100), in general, fertility should be assumed to be normal, and
all young women with type 1 diabetes should receive preconception counseling covering
diabetes and general topics, including use of prenatal vitamin, discontinuation of
potentially teratogenic medications, and the importance of glycemic control to reduce
the risk of congenital malformations.
Pregnancy
Type 1 diabetes affects approximately 0.1–0.2% of all pregnancies (101). During pregnancy,
there are substantial changes in maternal insulin sensitivity that may cause profound
changes in insulin requirements. Whereas insulin resistance increases markedly during
the second and third trimesters, a greater proportion of total daily insulin dose
must be given prandially and a lower proportion used to cover basal metabolic requirements
(102). Pregnant women with type 1 diabetes require meticulous glycemic management
by experts trained in obstetrics, endocrinology, and maternal-fetal medicine. Women
who are planning pregnancy or who are pregnant may need to test blood glucose levels
frequently (often 10 or more times daily) to reach and maintain a near-normal A1C
level without excessive hypoglycemia.
Severe hypoglycemia may occur early during pregnancy (102). This is followed by periods
of insulin resistance and subsequent hyperglycemia if the increased insulin needs
are not met. Therefore, health care providers must be vigilant and frequently adjust
insulin dosing throughout gestation.
In a pregnancy complicated by diabetes and chronic hypertension, target blood pressure
goals of systolic blood pressure 110–129 mmHg and diastolic blood pressure 65–79 mmHg
are reasonable. Lower blood pressure levels may be associated with impaired fetal
growth (Table 8). ACE inhibitors and angiotensin receptor blockers are contraindicated
during pregnancy because they may have adverse effects on the fetus. Antihypertensive
drugs known to be effective and safe in pregnancy include methyldopa, labetalol, diltiazem,
clonidine, and prazosin.
Table 8
ADA Standards of Care optimal targets in pregnancy*
Target maternal glucose†
Fasting
60–99 mg/dL
Peak postprandial
100–129 mg/dL
Mean
<100 mg/dL
Labor and delivery
80–110 mg/dL (mean <100)
Insulin drips + D10 50 cc/h
A1C
Preconception <7% and as close to normal as possible without significant hypoglycemia
During pregnancy <6%
*
See refs. 70, 103, and 104.
†
These represent the mean +2 SD for normal. They are targets, but not everyone can
achieve them. There is certainly marked variability, which explains why there is greater
incidence of large-for-gestational-age infants in patients with type 1 diabetes.
Eye examinations should occur in the first trimester with close follow-up throughout
pregnancy and for 1 year postpartum because of the risk of rapid retinopathy progression
during pregnancy. Those with progressive retinopathy should have more frequent screening
by an ophthalmologist experienced in retinopathy management. See the American Diabetes
Association/JDRF Type 1 Diabetes Sourcebook (70) for a summary of pregnancy recommendations.
The prevalence of Hashimoto thyroiditis may be as high as 31% in women with type 1
diabetes (105). Therefore, all pregnant women with type 1 diabetes should be screened
for thyroid disease early in pregnancy.
Recommendations
Starting at puberty, preconception counseling should be incorporated into routine
diabetes clinic visits for all adolescents and women of childbearing potential, and
appropriate birth control techniques should be discussed with women who do not desire
pregnancy. (C)
As most pregnancies are unplanned, consider the potential risks and benefits of medications
that are contraindicated in pregnancy in all adolescents and women of childbearing
potential and counsel women using such medications accordingly. (E)
Such medications should be evaluated prior to conception, as drugs commonly used to
treat diabetes and its complications may be contraindicated or not recommended in
pregnancy, including statins, ACE inhibitors, angiotensin receptor blockers, and most
noninsulin therapies. (B)
Prenatal vitamins with folate should be started with preconception planning to reduce
the risk for birth defects. (B)
All pregnant women with type 1 diabetes should be screened for thyroid disease early
in pregnancy. (B)
Women contemplating pregnancy should be evaluated and, if indicated, treated for diabetic
retinopathy, nephropathy, neuropathy, and CVD. (B)
A1C levels should be as close to normal as possible (<7%) before conception is attempted.
(B)
Nutritional intake should be optimized and included in preconception planning according
to general pregnancy guidelines. (E)
Inpatient Management and Outpatient Procedures
Management of individuals with type 1 diabetes in the hospital and in preparation
for scheduled outpatient procedures often differs from that of individuals with type
2 diabetes. The challenges include difficulties associated with fasting, maintaining
a consistent source of carbohydrate, and facilitating inpatient blood glucose management
while modifying scheduled insulin therapy. Outpatient procedures should be performed
with the awareness that individuals with type 1 diabetes may have difficulty fasting
for long periods of time (more than 10 h) prior to a procedure. Patients with type
1 diabetes should be prepared with a treatment plan for insulin dose adjustments and
oral glucose intake prior to any procedure that requires alterations in dietary intake
and/or fasting.
It is imperative that the entire health care team, including anesthesiologists and
surgeons as well as other specialists who perform procedures, understands type 1 diabetes
and how it factors into the comprehensive delivery of care. From a practical perspective,
this means that people with type 1 diabetes will be at high risk for hypoglycemia
during prolonged fasting and are at risk for ketosis if insulin is inappropriately
withheld. Once under anesthesia, individuals with type 1 diabetes must be carefully
monitored for hypoglycemia and hyperglycemia.
For some individuals, once the most acute phase of an illness has resolved or improved,
patients may be able to self-administer their prior multiple-dose or CSII insulin
regimen under the guidance of hospital personnel who are knowledgeable in glycemic
management. Individuals managed with insulin pumps and/or multiple-dose regimens with
carbohydrate counting and correction dosing may be allowed to manage their own diabetes
if this is what they desire, once they are capable of doing so.
Recommendations
All patients admitted to the hospital should have type 1 diabetes clearly identified
in the medical record. (E)
SMBG should be ordered to fit the patient’s usual insulin regimen with modifications
as needed based on clinical status. (E)
Goals for blood glucose levels are the same as for people with type 2 diabetes or
hospital-related hyperglycemia. (E)
A plan for preventing and treating hypoglycemia should be established for each patient.
(E)
Insulin dosing adjustments should be made in the perioperative period and inpatient
setting with consideration of changes in oral intake, recent blood glucose trends,
and the need for uninterrupted basal insulin to prevent hyperglycemia and ketoacidosis,
with adjustment of the long-acting insulin or basal insulin requirement to reflect
true basal requirements, insofar as they may be anticipated. (B)
Child Care and Schools
Because a large portion of a child’s day may be spent in school and/or in the child
care setting, close communication with and cooperation of the school or day care personnel
is essential for optimal diabetes management, safety, and maximal academic opportunities.
Child care personnel and school staff should receive training to provide diabetes
care in the absence of a school nurse or licensed health care professional. Able and
willing school staff members should be taught the principles of diabetes management
and trained to provide needed care for the child according to the ADA’s Safe at School
program (see the ADA position statement on diabetes care in the school and day care
setting [106] for further discussion). Young children often lack the motor, cognitive,
and communication skills and abilities to manage their diabetes and completely depend
on adult caregivers. The management priority for younger children is the prevention,
recognition, and treatment of hypoglycemia and marked hyperglycemia.
Students with diabetes should receive proper diabetes management in school, with as
little disruption to the school and child’s routine as possible. Whenever possible,
the student should have the opportunity to self-manage by performing blood glucose
monitoring, using CGM (if utilized), administering insulin, having access to meals/snacks,
managing hypoglycemia (with trained personnel prepared to provide glucagon treatment,
if required) and hyperglycemia, and participating fully in all school-sponsored activities
(Table 9).
Table 9
Diabetes care tasks for school personnel
Diabetes care tasks
Signs*
Treatment
Outcome if not treated
Hypoglycemia recognition and treatment
Catecholamine effect (sweating, jitteriness, tachycardia, and palpitations) or neuroglycopenia
(behavior change)
Glucose, wait 15 min, recheck, give food if blood glucose is adequate (based on DMMP)
Seizure or coma
Know when and how to give glucagon
Know when to contact parents or emergency medical services
Have all contact information available on emergency plan
Hyperglycemia recognition and treatment
Polyuria, polydipsia (most common), difficulty concentrating, headache, or irritability
Rapid- or short-acting insulin
Check for ketones. Follow directions for ketones if positive to avoid ketoacidosis
Dose and frequency should be clearly elucidated on emergency plan to avoid “insulin
stacking” and consequent hypoglycemia (DMMP)
Insulin dosing technique (syringe/vial, pens, pumps)
Insulin required (DMMP)
Ketone checks and when to call parents
Correction factor calculations and insulin for hyperglycemia and ketones
DMMP, Diabetes Medical Management Plan.
*
Varies among individuals but consistent within a given child.
Camps
A diabetes camp is an ideal place for children and youth to have an enjoyable camp
experience and receive peer support from other children with diabetes under close
medical oversight. The goals for campers are to learn to cope more effectively with
diabetes, learn self-management skills to gain more independence, and share experiences
with other young people with diabetes.
The camp medical director is responsible for the diabetes management of the children.
A registered dietitian oversees dietary planning at camp. Medical directors and staff
should have expertise in managing type 1 diabetes and must receive training concerning
routine diabetes management and treatment of diabetes-related emergencies at camp.
Staff must follow universal precautions including Occupational Safety and Health Administration
(OSHA) regulations, Clinical Laboratory Improvement Amendments (CLIA) standards, and
state regulations (107).
Diabetes in the Workplace
There are practical and legal issues related to diabetes in the workplace. Employers
and employees with diabetes should work together to find solutions and educate themselves
about the rights of individuals with diabetes. Individuals with diabetes are responsible
for having all necessary diabetes supplies, eating properly, and being aware of safety
issues and regulations at work. The Americans with Disabilities Act states that most
employers must provide “reasonable accommodations” to allow an individual with diabetes
to safely and successfully perform a job, unless doing so would place an “undue burden”
on the employer. We refer the reader to ADA position statement on diabetes and employment
for additional information (108) and to the relevant section of the American Diabetes
Association/JDRF Type 1 Diabetes Sourcebook (70).
Older Adults
Older individuals with type 1 diabetes are unique in that they have lived for many
years with a complex disease. Not all older adults are alike: some may continue a
rigorous regimen, with tighter control, while others may require less stringent targets.
Along with age-related conditions, older adults may develop diabetes-related complications,
which make managing type 1 diabetes more challenging. Providers should be aware that
insulin dosing errors, meal planning, and physical activities must be properly managed
in older adults. Severe hyperglycemia can lead to symptoms of dehydration and hyperglycemic
crises. While chronic hyperglycemia is detrimental, hypoglycemia may be more of a
concern in some older adults. Declining cognition may contribute to hypoglycemia unawareness
or the inability to safely manage hypoglycemia when it occurs. An individualized approach
that includes the reassessment of prior targets may be warranted. We refer the reader
to the ADA consensus report “Diabetes in Older Adults” (54). Even though this report
focuses primarily on the type 2 diabetic population, there is significant overlap
in the comorbidities and complications experienced by the older type 1 and type 2
diabetic populations.
Special Population Groups
Although type 1 diabetes is increasing in several ethnic and racial groups, it remains
less common in people of non-European descent. A better understanding of the unique
pathophysiology of type 1 diabetes is needed. In addition, multidisciplinary diabetes
teams should receive training to properly address the diverse cultural needs of these
populations and to optimize health care delivery, improve glycemic control, and prevent
complications. Additionally, there is a need for approaches to reduce health disparities
and improve outcomes in racial/ethnic minorities and in the underserved population
with type 1 diabetes (70).
Developing Countries: The Global Epidemic
Type 1 diabetes is an increasing global public health burden. The demands of daily
management, chronicity of the disease, potential complications, paucity of diabetes
specialists, and rising incidence are challenging in the U.S., but these issues, including
the considerable cost of management, are crippling for those in the developing world.
International organizations play a major role in improving care for individuals with
type 1 diabetes in the developing world, but implementable, cost-saving, and sustainable
strategies are needed to make such programs successful (70).
Related collections
Most cited references68
- Record: found
- Abstract: found
- Article: not found
The cation efflux transporter ZnT8 (Slc30A8) is a major autoantigen in human type 1 diabetes.
Janet Wenzlau, Kirstine Juhl, Liping Yu … (2007)
- Record: found
- Abstract: found
- Article: not found
MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial.
Rory Collins, Jane Armitage, Sarah Parish … (2003)