- Record: found
- Abstract: found
- Article: found
Hyperuricemia and its related histopathological features on renal biopsy
Read this article at
Abstract
Background
Hyperuricemia (HUA) is very common in chronic kidney disease (CKD). HUA is associated with an increased risk of cardiovascular events and accelerates the progression of CKD. Our study aimed to explore the relationship between baseline serum uric acid levels and renal histopathological features.
Methods
One thousand seventy patients receiving renal biopsy in our center were involved in our study. The baseline characteristics at the time of the kidney biopsy were collected from Renal Treatment System (RTS) database, including age, gender, serum uric acid (UA), glomerular filtration rate (eGFR), serum creatinine (Cr), urea, albumin (Alb), 24 h urine protein quantitation (24 h-u-pro) and blood pressure (BP). Pathological morphological changes were evaluated by two pathologists independently. Statistical analysis was done using SPSS 21.0.
Results
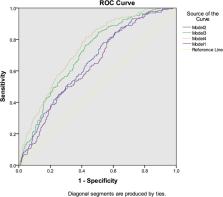
Among 1070 patients, 429 had IgA nephropathy (IgAN), 641 had non-IgAN. The incidence of HUA was 38.8% ( n = 415), 43.8% ( n = 188), and 43.2% ( n = 277) in all patients, patients with IgAN and non-IgAN patients, respectively. Serum uric acid was correlated with eGFR ( r = − 0.418, p < 0.001), Cr ( r = 0.391, p < 0.001), urea ( r = 0.410, p < 0.001), 24-u-pro ( r = 0.077, p = 0.022), systolic blood pressure (SBP) ( r = 0.175, p < 0.001) and diastolic blood pressure (DBP) ( r = 0.109, p = 0.001). Multivariate logistic regression analysis showed that after adjustment for Cr, age and blood pressure, HUA was a risk factor for segmental glomerulosclerosis (OR = 1.800, 95% CI:1.309–2.477) and tubular atrophy/interstitial fibrosis (OR = 1.802, 95% CI:1.005–3.232). HUA increased the area under curve (AUC) in diagnosis of segmental glomerulosclerosis.
Related collections
Most cited references23

- Record: found
- Abstract: found
- Article: found
Prevalence of Hyperuricemia and Gout in Mainland China from 2000 to 2014: A Systematic Review and Meta-Analysis
- Record: found
- Abstract: found
- Article: not found
Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system.
- Record: found
- Abstract: found
- Article: not found