- Record: found
- Abstract: found
- Article: found
Primary Thyroid Extranasal NK/T-Cell Lymphoma Associated With Good Outcome: A Case Report and Literature Review : A Care-Compliant Article
Read this article at
Abstract
Most thyroid lymphomas are B-lineage, and T-cell lymphomas are rare. None of primary thyroid extranasal NK/T-cell lymphoma (NKTCL) has been reported in the literature. Here, we report a case of extranasal NKTCL exclusively arising in the thyroid in an 18-year-old Chinese.
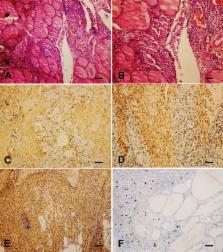
The patient presented with rapid anterior swelling at the neck and aggravated dyspnea for 2 months. Neck computer tomography scan revealed diffuse thyroid enlargement in the left lobe compressing the trachea. The thyroid function test was indicative of hypothyroidism. Gastroscopy demonstrated chronic nonspecific gastritis. Subtotal thyroidectomy was performed. Histological examination showed a diffuse infiltration of neoplastic lymphoid cells with an angiodestructive behavior. Immunophenotype is positive for CD2, CD56, CD43, and TIA-1, and typically negative for surface CD3. Epstein-Barr virus-encoded small RNAs were detected in tumor cells. A diagnose of primary thyroid extranasal NKTCL-N lymphoma was confirmed by the findings.
The patient was treated with CHOP-L combination chemotherapy followed by local radiotherapy, and tolerated the modality well. The patient has been in remission for 28 months so far.
To our knowledge, this is the first case report of primary extranasal NKTCL exclusively arising in the thyroid. The case has a relatively good treatment outcome with timely diagnosis and multimodality approach.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project.
- Record: found
- Abstract: found
- Article: not found