- Record: found
- Abstract: found
- Article: found
Optimising drug prescribing and dispensing in subjects at risk for drug errors due to renal impairment: improving drug safety in primary healthcare by low eGFR alerts
Read this article at
Abstract
Objectives
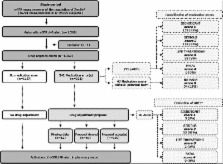
To assess the risk of medication errors in subjects with renal impairment (defined as an estimated glomerular filtration rate (eGFR) ≤40 ml/min/1.73 m 2) and the effectiveness of automatic eGFR ≤40-alerts relayed to community pharmacists.
Setting
The city of Zwolle, The Netherlands, in a primary care setting including 22 community pharmacists and 65 general practitioners.
Participants
All adults who underwent ambulatory creatine measurements which triggered an eGFR ≤40-alert.
Primary and secondary outcome measures
The total number of ambulatory subjects with an eGFR ≤40-alert during the study period of 1 year and the number of medication errors related to renal impairment. The type and number of proposed drug adjustments recommended by the community pharmacist and acceptance rate by the prescribing physicians. Classification of all medication errors on their potential to cause an adverse drug event (ADE) and the actual occurrence of ADEs (limited to those identified through hospital record reviews) 1 year after the introduction of the alerts.
Results
Creatine measurements were performed in 25 929 adults. An eGFR ≤40-alert was indicated for 5.3% (n=1369). This group had a median (IQR) age of 78 (69, 84) years, and in 73% polypharmacy (≥5 drugs) was present. In 15% (n=211) of these subjects, a medication error was detected. The proportion of errors increased with age. Pharmacists recommended 342 medication adjustments, mainly concerning diuretics (22%) and antibiotics (21%). The physicians’ acceptance rate was 66%. Of all the medication errors, 88% were regarded as potential ADEs, with most classified as significant or serious. At follow-up, the ADE risk (n=40) appeared highest when the proposed medication adjustments were not implemented (38% vs 6%).
Conclusions
The introduction of automatic eGFR-alerts identified a considerable number of subjects who are at risk for ADEs due to renal impairment in an ambulatory setting. The nationwide implementation of this simple protocol could identify many potential ADEs, thereby substantially reducing iatrogenic complications in subjects with impaired renal function.
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
Incidence and preventability of adverse drug events among older persons in the ambulatory setting.
- Record: found
- Abstract: found
- Article: not found
Adverse drug events in ambulatory care.
- Record: found
- Abstract: found
- Article: not found