- Record: found
- Abstract: found
- Article: found
Medication adherence in chronic illness: do beliefs about medications play a role?
Abstract
Background
Several medicines are prescribed for chronic disease management; however, adherence to long-term therapy remains poor. Culture influences beliefs about medications and, ultimately, adherence to treatment. There is a paucity of data with regard to beliefs about medications in the Middle East region, and it remains to be determined how these beliefs would impact treatment adherence.
Objectives
To investigate the relationship between patients’ beliefs about medications with self-reported adherence to treatment among a chronically ill multicultural patient population.
Methods
A prospective cross-sectional study was conducted among patients treated for chronic illnesses in the Ministry of Health primary care clinics in Kuwait. Patients completed a questionnaire that consisted of questions to collect information about their health status and demographics using validated instruments: the Beliefs about Medication, Sensitive Soma Assessment Scale, and Medication Adherence Report Scale-5 items. The main outcome measures were self-reported adherence to medications, beliefs, and perceived sensitivity toward medications.
Results
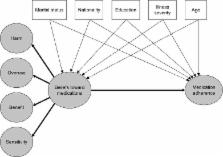
Of the 1,150 questionnaires distributed, 783 were collected – giving a response rate of 68.1%. Of the 783 patients, 56.7% were male, 73.7% were married, 53.3% were non-Kuwaitis, and 49.4% had low income (<1,000 KD/3,350 USD monthly). Patients self-reported having a cardiovascular illness (80.2%), diabetes mellitus (67.7%), respiratory disease (24.3%), or mood disorder (28.6%). Participants had a mean of two comorbid illnesses and indicated taking an average of four prescription medicines to treat them. A structural equation model analysis showed adherence to medications was negatively impacted by higher negative beliefs toward medications (beta = −0.46). Factors associated with negative beliefs toward medications included marital status (being unmarried; beta = −0.14), nationality (being Kuwaiti; beta = 0.15), having lower education level (beta = −0.14), and higher illness severity (beta = 0.15). Younger age (beta = 0.10) and higher illness severity (beta = −0.9) were independently associated with lower medication adherence. Income and gender did not influence medication adherence or beliefs about medications. The combined effect of variables tested in the model explained 24% of the variance in medication adherence.
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Patient adherence to treatment: three decades of research. A comprehensive review.
- Record: found
- Abstract: found
- Article: not found
Primary medication non-adherence: analysis of 195,930 electronic prescriptions.
- Record: found
- Abstract: found
- Article: not found