- Record: found
- Abstract: found
- Article: found
Impact of the Comorbidity Polypharmacy Score on Clinical Outcome in Patients with Hip Fracture undergoing surgery Using Real-World Data
Read this article at
ABSTRACT
BACKGROUND
The Comorbidity Polypharmacy Score (CPS) is calculated by the number of drugs carried plus the number of comorbidities on admission and divided into three categories (minor, 0–7; moderate, 8–14; and severe, 15+). This study investigates whether CPS can predict the clinical outcomes in older patients with hip fractures undergoing surgery.
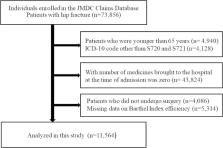
METHODS
This retrospective longitudinal study used a multicenter hospital-based database containing the Diagnosis Procedure Combination. Consecutive patients with hip fractures (ICD-10 codes S720 and S721) who were aged ≥65 years between April 2014 and August 2020 were included. We evaluated the predictive association between the CPS and Barthel Index (BI) efficiency. The primary outcome was defined as the BI efficiency, and the secondary outcome was the length of hospital stay.
RESULTS
We enrolled 11,564 patients, and 80.5% of them were female. The mean age was 83.9 ± 6.5 years. The BI efficiency was the lowest in the CPS severe group with a median [interquartile range] of 0.67 [0.10, 1.43]. The length of hospital stay was the highest in the CPS severe group, with a median of 35 [21, 58]. Additionally, multiple linear regression analysis revealed that the CPS was independently associated with the BI efficiency (β = −0.100, 95% CI: −0.040, −0.029; P < 0.001) and the length of hospital stay (β = 0.047, 95% CI: 0.199, 0.366; P < 0.001).
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Comorbidity-polypharmacy scoring facilitates outcome prediction in older trauma patients.
- Record: found
- Abstract: found
- Article: not found
The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients.

- Record: found
- Abstract: found
- Article: found