- Record: found
- Abstract: found
- Article: found
SGLT-2 receptor inhibitors for treating patients with type 2 diabetes mellitus: a systematic review and network meta-analysis
Read this article at
Abstract
Objective
Because of the lack of head-to-head trials, the aim was to indirectly compare sodium glucose transporter-2 (SGLT-2) inhibitors in the treatment of type 2 diabetes.
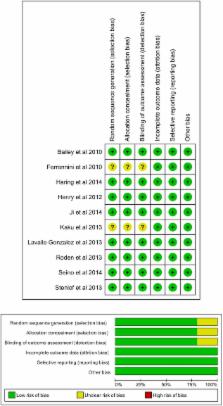
Eligibility criteria
Randomised controlled trials assessing the efficacy of SGLT-2 inhibitors in patients with type 2 diabetes inadequately controlled with diet and exercise alone or metformin monotherapy. Minimum duration 24 weeks. Indirect comparison was undertaken using Bayesian methods.
Results
In monotherapy, a greater proportion of patients achieved a glycated haemoglobin (HbA1c) level of <7% on canagliflozin 300 mg than on canagliflozin 100 mg (risk ratio (RR) 0.72%, 95% credible intervals (CrI) 0.59% to 0.87%) and dapagliflozin 10 mg (RR 0.63, 95% CrI 0.48 to 0.85) but there were no significant differences compared with either dose of empagliflozin. In monotherapy, canagliflozin 300 mg reduced HbA1c more than other SGLT-2 inhibitors (mean difference ranged from 0.20% to 0.64%). There were no significant differences in weight reduction. All the flozins reduced systolic blood pressure (SBP) more than placebo, ranging from a reduction of 6 mm Hg with canagliflozin 300–2.6 mm Hg with empagliflozin 10 mg. In dual therapy with metformin, all flozins were more effective than placebo for achieving HbA1c <7%, and reducing HbA1c, weight and SBP. The proportions achieving HbA1c level of <7% were mostly similar. Canagliflozin 300 mg reduced HbA1c more than the other drugs but this just reached statistical significance only against canagliflozin 100 mg (MD 0.15, CrI 0.04 to 0.26).
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin.
- Record: found
- Abstract: found
- Article: not found
Euglycemic Diabetic Ketoacidosis: A Potential Complication of Treatment With Sodium–Glucose Cotransporter 2 Inhibition
- Record: found
- Abstract: found
- Article: not found