- Record: found
- Abstract: found
- Article: not found
An Orthopedic-Hospitalist Comanaged Hip Fracture Service Reduces Inpatient Length of Stay
Read this article at
Abstract
Introduction:
Hip fractures are common in the elderly patients with an incidence of 320 000 fractures/year in the United States, representing a health-care cost of US$9 to 20 billion. Hip fracture incidence is projected to increase dramatically. Hospitals must modify clinical models to accommodate this growing burden. Comanagement strategies are reported in the literature, but few have addressed orthopedic-hospitalist models. An orthopedic-hospitalist comanagement (OHC) service was established at our hospital to manage hip fracture patients. We sought to determine whether the OHC (1) improves the efficiency of hip fracture management as measured by inpatient length of stay (LOS) and time to surgery (TTS) and (2) whether our results are comparable to those reported in hip fracture comanagement literature.
Methods:
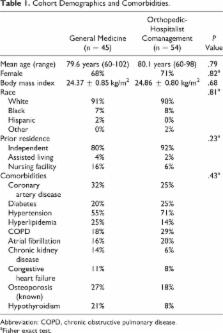
A comparative retrospective–prospective cohort study of patients older than 60 years with an admitting diagnosis of hip fracture was conducted to compare inpatient LOS and TTS for hip fracture patients admitted 10 months before (n = 45) and 10 months after implementation (n = 54) of the OHC at a single academic hospital. Secondary outcome measures included percentage of patients taken to surgery within 24 or 48 hours, 30-day readmission rates, and mortality. Outcomes were compared to comanagement study results published in MEDLINE-indexed journals.
Results:
Patient cohort demographics and comorbidities were similar. Inpatient LOS was reduced by 1.6 days after implementation of the OHC ( P = .01) without an increase in 30-day readmission rates or mortality. Time to surgery was insignificantly reduced from 27.4 to 21.9 hours ( P = .27) and surgery within 48 hours increased from 86% to 96% ( P = .15).
Related collections
Most cited references26

- Record: found
- Abstract: found
- Article: found
Timing Matters in Hip Fracture Surgery: Patients Operated within 48 Hours Have Better Outcomes. A Meta-Analysis and Meta-Regression of over 190,000 Patients
- Record: found
- Abstract: found
- Article: not found
Association of timing of surgery for hip fracture and patient outcomes.
- Record: found
- Abstract: found
- Article: not found
