- Record: found
- Abstract: found
- Article: found
DSM265 for Plasmodium falciparum chemoprophylaxis: a randomised, double blinded, phase 1 trial with controlled human malaria infection
Read this article at
Summary
Background
A drug for causal (ie, pre-erythrocytic) prophylaxis of Plasmodium falciparum malaria with prolonged activity would substantially advance malaria control. DSM265 is an experimental antimalarial that selectively inhibits the parasite dihydroorotate dehydrogenase. DSM265 shows in vitro activity against liver and blood stages of P falciparum. We assessed the prophylactic activity of DSM265 against controlled human malaria infection (CHMI).
Methods
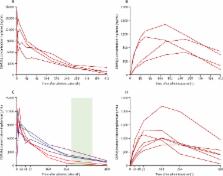
At the Institute of Tropical Medicine, Eberhard Karls University (Tübingen, Germany), healthy, malaria-naive adults were allocated to receive 400 mg DSM265 or placebo either 1 day (cohort 1A) or 7 days (cohort 2) before CHMI by direct venous inoculation (DVI) of 3200 aseptic, purified, cryopreserved P falciparum sporozoites (PfSPZ Challenge; Sanaria Inc, Rockville, MD, USA). An additional group received daily atovaquone-proguanil (250-100 mg) for 9 days, starting 1 day before CHMI (cohort 1B). Allocation to DSM265, atovaquone-proguanil, or placebo was randomised by an interactive web response system. Allocation to cohort 1A and 1B was open-label, within cohorts 1A and 2, allocation to DSM265 and placebo was double-blinded. All treatments were given orally. Volunteers were treated with an antimalarial on day 28, or when parasitaemic, as detected by thick blood smear (TBS) microscopy. The primary efficacy endpoint was time-to-parasitaemia, assessed by TBS. All participants receiving at least one dose of chemoprophylaxis or placebo were considered for safety, those receiving PfSPZ Challenge for efficacy analyses. Log-rank test was used to compare time-to-parasitemia between interventions. The trial was registered with ClinicalTrials.gov, number NCT02450578.
Findings
22 participants were enrolled between Oct 23, 2015, and Jan 18, 2016. Five participants received 400 mg DSM265 and two participants received placebo 1 day before CHMI (cohort 1A), six participants received daily atovaquone-proguanil 1 day before CHMI (cohort 1B), and six participants received 400 mg DSM265 and two participants received placebo 7 days before CHMI (cohort 2). Five of five participants receiving DSM265 1 day before CHMI and six of six in the atovaquone-proguanil cohort were protected, whereas placebo recipients (two of two) developed malaria on days 11 and 14. When given 7 days before CHMI, three of six volunteers receiving DSM265 became TBS positive on days 11, 13, and 24. The remaining three DSM265-treated, TBS-negative participants of cohort 2 developed transient submicroscopic parasitaemia. Both participants receiving placebo 7 days before CHMI became TBS positive on day 11. The only possible DSM265-related adverse event was a moderate transient elevation in serum bilirubin in one participant.
Related collections
Most cited references12
- Record: found
- Abstract: found
- Article: not found
Sterile protection against human malaria by chemoattenuated PfSPZ vaccine
- Record: found
- Abstract: found
- Article: not found
Illness in travelers visiting friends and relatives: a review of the GeoSentinel Surveillance Network.

- Record: found
- Abstract: found
- Article: found