- Record: found
- Abstract: found
- Article: found
Evaluation of Singh Index and Osteoporosis Self-Assessment Tool for Asians as risk assessment tools of hip fracture in patients with type 2 diabetes mellitus
Read this article at
Abstract
Background
Type 2 diabetes mellitus (T2DM), an epidemic disease around world, has recently been identified as a risk factor for osteoporosis-associated fracture. However, there is no consensus on the best method of assessing fracture risk in patients with T2DM. The aim of this study was to evaluate the usefulness of the Osteoporosis Self-Assessment Tool for Asians (OSTA) and the Singh Index (SI) in hip fracture risk assessment in patients with T2DM.
Methods
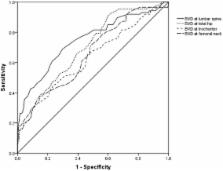
We enrolled 261 postmenopausal women with T2DM: 87 had hip fracture resulting from low-energy trauma and 174 age-matched controls had no fracture (two controls per fracture case). Bone mineral density (BMD) was measured with dual-energy X-ray absorptiometry in the lumbar spine and hip region. The SI was obtained from standard antero-posterior radiographs of the pelvis. The OSTA was calculated with a formula based on weight and age. Data were analyzed with descriptive statistics and tests of difference. Receiver operating characteristic analysis was used to determine optimum cutoff values, sensitivity, and specificity of screening methods. Discriminative abilities of different screening tools were compared with the area under the curve (AUC).
Results
There were significant differences in BMD at all sites (lumbar spine, femoral neck, trochanter, and total hip) and in SI between the fracture and non-fracture groups ( P < 0.05). There was no significant difference in OSTA between the groups ( P > 0.05). The area under the curve was 0.747 (95% CI: 0.680–0.813) for lumbar spine BMD, 0.699 (95% CI: 0.633–0.764) for total hip BMD, 0.659 (95% CI: 0.589–0.729) for femoral neck BMD, 0.631 (95% CI: 0.557–0.704) for trochanter BMD, 0.534 (95% CI: 0.459–0.610) for OSTA, 0.636 (95% CI: 0.564–0.709) for SI, and 0.795 (95% CI: 0.734–0.857) for OSTA plus SI. The AUC for combined OSTA plus SI was significantly superior to other parameters besides BMD of the lumbar spine.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes.
- Record: found
- Abstract: found
- Article: not found
High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus.
- Record: found
- Abstract: found
- Article: not found