- Record: found
- Abstract: found
- Article: found
Depression in the Elderly. Consensus Statement of the Spanish Psychogeriatric Association
Read this article at
Abstract
Introduction
Present knowledge about depression in the elderly is still scarce and often controversial, despite its high frequency and impact. This article reports the results and most relevant conclusions of a Delphi-based consensus on geriatric depression promoted by the Spanish Psychogeriatric Association.
Methods
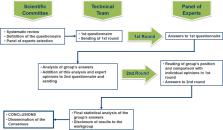
A 78-item questionnaire was developed by 7 highly specialized geriatric psychiatrists and was evaluated using the Modified Delphi technique in two rounds answered by 35 psychiatrists with an extensive expertise in geriatric depression. The topics and number of questions (in brackets) covered were: concepts, clinical aspects, and risk factors (12); screening and diagnosis (7); psychotic depression (17); depression and dementia (5); antidepressant drug treatment (18); non-pharmacological biological treatments (5); psychotherapeutic treatments (4); comorbidity and preventive aspects (6); professional training needed (4). In addition, the expert panel’s opinion on the antidepressants of choice in 21 common comorbid conditions and on different strategies to approach treatment-resistant cases in terms of both efficacy and safety was assessed.
Results
After the two rounds of the Delphi process, consensus was reached for 59 (75.6%) of the 78 items. Detailed recommendations are included in the text. Considering pharmacological treatments, agomelatine was the most widely mentioned drug to be recommended in terms of safety in comorbid conditions. Desvenlafaxine, sertraline, and vortioxetine, were the most frequently recommended antidepressants in comorbid conditions in general. Combining parameters of efficacy and safety, experts recommended the following steps to address cases of treatment resistance: 1. Escalation to the maximum tolerated dose; 2. Change of antidepressant; 3. Combination with another antidepressant; 4. Potentiation with an antipsychotic or with lamotrigine; 5. Potentiation with lithium; 6. Potentiation with dopamine agonists or methylphenidate
Discussion and Conclusions
Consensus was reached for a high number of items as well as for the management of depression in the context of comorbid conditions and in resistant cases. In the current absence of sufficient evidence-based information, our results can be used to inform medical doctors about clinical recommendations that might reduce uncertainty in the diagnosis and treatment of elderly patients with depressive disorders.
Related collections
Most cited references91
- Record: found
- Abstract: found
- Article: not found
Management of Depression in Older Adults: A Review.
- Record: found
- Abstract: found
- Article: not found
Neuropsychiatric predictors of progression from amnestic-mild cognitive impairment to Alzheimer's disease: the role of depression and apathy.
- Record: found
- Abstract: not found
- Article: not found