- Record: found
- Abstract: found
- Article: found
Different scan areas affect the detection rates of diabetic retinopathy lesions by high-speed ultra-widefield swept-source optical coherence tomography angiography
Read this article at
Abstract
Introduction
The study aimed to determine the effect of the scanning area used for high-speed ultra-widefield swept-source optical coherence tomography angiography (SS-OCTA) on the detection rate of diabetic retinopathy (DR) lesions.
Methods
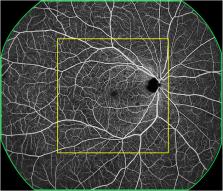
This prospective, observational study involved diabetic patients between October 2021 and April 2022. The participants underwent a comprehensive ophthalmic examination and high-speed ultra-widefield SS-OCTA using a 24 mm × 20 mm scanning protocol. A central area denoted as “12 mm × 12 mm-central” was extracted from the 24 mm × 20 mm image, and the remaining area was denoted as “12 mm~24mm-annulus.” The rates of detection of DR lesions using the two scanning areas were recorded and compared.
Results
In total, 172 eyes (41 eyes with diabetes mellitus without DR, 40 eyes with mild to moderate non-proliferative diabetic retinopathy (NPDR), 51 eyes with severe NPDR, and 40 eyes with proliferative diabetic retinopathy (PDR) from 101 participants were included. The detection rates of microaneurysms (MAs), intraretinal microvascular abnormalities (IRMAs), and neovascularization (NV) for the 12 mm × 12 mm central and 24 mm × 20 mm images were comparable (p > 0.05). The detection rate of NPAs for the 24 mm × 20 mm image was 64.5%, which was significantly higher than that for the 12 mm × 12 mm central image (52.3%, p < 0.05). The average ischemic index (ISI) was 15.26% for the 12 mm~24mm-annulus, which was significantly higher than that for the 12 mm × 12 mm central image (5.62%). Six eyes had NV and 10 eyes had IRMAs that only existed in the 12 mm~24mm-annulus area.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: found
Global Prevalence and Major Risk Factors of Diabetic Retinopathy
- Record: found
- Abstract: found
- Article: not found
Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales.
- Record: found
- Abstract: found
- Article: not found