- Record: found
- Abstract: found
- Article: found
Thiamine responsive megaloblastic anemia syndrome associated with patent ductus arteriosus: First case report from Kashmir Valley of the Indian subcontinent
Read this article at
Abstract
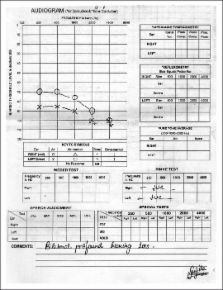
Thiamine responsive megaloblastic anemia syndrome, an autosomal recessive inherited disorder characterized by a triad of anemia, diabetes mellitus and sensorineural deafness is caused by a deficiency of a thiamine transporter protein. The disorder is rare and has not been reported from our community which has high background of consanguinity. We report a six years old girl who presented with diabetes mellitus which remitted after thiamine replacement. The girl in addition had sensorineural deafness, reinopathy, atrial septal defect and megaloblastic anemia which responded to high doses of thymine. This is the first case reported from Kashmir valley and third from India. The presentation and management in such cases is discussed.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Mutations in a new gene encoding a thiamine transporter cause thiamine-responsive megaloblastic anaemia syndrome.
- Record: found
- Abstract: not found
- Article: not found
Thiamine-responsive megaloblastic anemia.
- Record: found
- Abstract: found
- Article: not found