- Record: found
- Abstract: found
- Article: found
Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture
Read this article at
Abstract
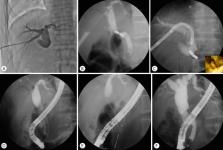
A number of different conditions can lead to a bile duct stricture. These strictures are particularly common after biliary operations, including living-donor liver transplantation. Endoscopic and percutaneous methods have high success rates in treating benign biliary strictures. However, these conventional methods are difficult to manage when a guidewire cannot be passed through areas of severe stenosis or complete obstruction. Magnetic compression anastomosis has emerged as an alternative nonsurgical treatment method to avoid the mortality and morbidity risks of reoperation. The feasibility and safety of magnetic compression anastomosis have been reported in several experimental and clinical studies in patients with biliobiliary and bilioenteric strictures. Magnetic compression anastomosis is a minimally traumatic and highly effective procedure, and represents a new paradigm for benign biliary strictures that are difficult to treat with conventional methods.
Related collections
Most cited references71
- Record: found
- Abstract: not found
- Article: not found
An analysis of the problem of biliary injury during laparoscopic cholecystectomy.
- Record: found
- Abstract: found
- Article: not found
Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective.
- Record: found
- Abstract: found
- Article: not found