- Record: found
- Abstract: found
- Article: found
Simply modified percutaneous tracheostomy using the Cook® Ciaglia Blue Rhino™: a case series
Read this article at
Abstract
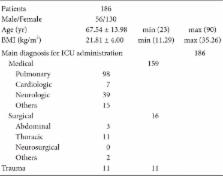
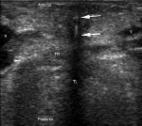
When first introduced, percutaneous dilatational tracheostomy (PDT) was performed using a bronchoscope. The bronchoscope itself, however, has several disadvantages, including interruption of ventilation. Modifications of the standard PDT technique have suggested that PDT can be safely performed without a bronchoscope. However, the safety of these modifications is unclear and many modifications have yet to be widely adopted. This study retrospectively evaluated the safety of a simplified PDT technique using the Cook® Ciaglia Blue Rhino™ in 186 patients. After confirming the underlying structures by palpation, PDT was performed without a bronchoscope or blunt dissection, 2.0 cm below the cricothyroid membrane. Ultrasonography was used only when palpation was difficult. Except for bleeding in three patients with coagulopathy, none of the patients experienced any early or late complications, and there were no deaths related to PDT. These findings confirm that PDT can be safely performed using a simplified technique, which may be useful in situations with limited equipment and medical personnel.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Percutaneous tracheostomy: ciaglia blue rhino versus the basic ciaglia technique of percutaneous dilational tracheostomy.
- Record: found
- Abstract: found
- Article: found
Ultrasound-guided percutaneous tracheostomy in critically ill obese patients
- Record: found
- Abstract: found
- Article: not found