- Record: found
- Abstract: found
- Article: found
Aquaporin-4 IgG antibodies: predictors of positivity and their relationship with neuropsychiatric disorders and white matter lesions in Juvenile systemic lupus erythematosus
Read this article at
Abstract
Background
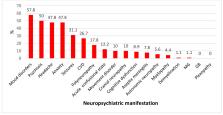
This study aimed to describe the prevalence of the various clinical features and severity of juvenile systemic lupus erythematosus (jSLE) and to assess predictors of AQP4-Ab positivity in jSLE. In addition, we assessed the relationship of AQP4-Abs with neuropsychiatric disorders and white matter lesions in jSLE.
Method
For 90 patients with jSLE, demographic data, clinical manifestations, and treatments received were recorded, and all of the patients were underwent clinical examinations, including assessments for the neurological manifestations of jSLE and neuropsychiatric disorders; Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score evaluations; laboratory investigations, including serum AQP4-Ab assays; and 1.5 Tesla brain MRI. Echocardiography and renal biopsy were performed for the indicated patients.
Result
Fifty-six patients (62.2%) tested positive for AQP4-Abs. These patients were more likely to have higher disease activity scores (p < 0.001); discoid lesions (p = 0.039); neurological disorders (p = 0.001), mainly psychosis and seizures (p = 0.009 and p = 0.032, respectively); renal and cardiac involvement (p = 0.004 and p = 0.013, respectively); lower C3 levels (p = 0.006); white matter hyperintensities (p = 0.008); and white matter atrophy (p = 0.03) than patients who were negative for AQP4-Abs. Furthermore, AQP4-Ab-positive patients were more likely to have received cyclophosphamide (p = 0.028), antiepileptic drugs (p = 0.032) and plasma exchange therapy (p = 0.049).
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Systemic lupus erythematosus disease activity index 2000.
- Record: found
- Abstract: found
- Article: not found
2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus
- Record: found
- Abstract: found
- Article: not found