- Record: found
- Abstract: found
- Article: found
Complete response of mediastinal clear cell sarcoma to pembrolizumab with radiotherapy
Read this article at
Abstract
Background
Clear cell sarcoma (CCS) is a rare, aggressive soft tissue sarcoma thought to derive from neural crest and characterized by a 12;22 translocation. The resulting fusion protein directly activates expression of the melanocyte master transcription factor and drives the same down-stream pathways in CCS and melanoma leading to significant clinical parallels between these malignancies. Striking success of immune checkpoint blockade in melanoma has promoted interest in immunotherapy of CCS.
Case presentation
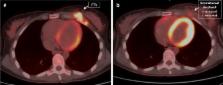
We report the first complete clinical response of a bulky chest wall recurrence of mediastinal CCS in a young woman to anti-PD1 checkpoint blockade with pembrolizumab combined with standard fractionation radiotherapy to enhance regional control and potentially boost the systemic immune response. The treatment was well tolerated with grade 2 skin toxicity within the range expected with radiation alone. Significant reduction in tumor bulk occurred after only 2 radiation fractions and complete response was achieved at 50 Gray.
Conclusion
The complete clinical response observed in our patient suggests synergy between concurrent radiotherapy and PD1 blockade in CCS. This case and the striking parallels between CCS and melanoma indicate the need for prospective trials of immune checkpoint blockade combined with radiotherapy in this rare malignancy.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Radiotherapy and immunotherapy: a beneficial liaison?
- Record: found
- Abstract: found
- Article: not found
Efficacy and Safety of Nivolumab Alone or in Combination With Ipilimumab in Patients With Mucosal Melanoma: A Pooled Analysis.
- Record: found
- Abstract: found
- Article: not found