- Record: found
- Abstract: found
- Article: found
Prediction of multivessel coronary artery disease and candidates for stress-only imaging using multivariable models with myocardial perfusion imaging
Read this article at
Abstract
Purpose
Selecting patients with coronary multivessel disease (MVD) or no stenosis using myocardial perfusion imaging (MPI) is challenging. We aimed to create a model to predict MVD using a combination of quantitative MPI values and background factors of patients. We also assessed whether patients in the same database could be selected who do not require rest studies (stress-only imaging).
Methods
We analyzed data from 1001 patients who had been assessed by stress MPI at 12 centers and 463 patients who had not undergone revascularization in Japan. Quantitative values based on MPI were obtained using cardioREPO software, which included myocardial perfusion defect scores, left ventricular ejection fractions and volumes. Factors in MPI and clinical backgrounds that could predict MVD were investigated using univariate and multivariate analyses. We also investigated whether stress data alone could predict patients without coronary stenosis to identify candidates for stress-only imaging.
Results
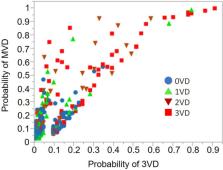
We selected summed stress score (SSS), rest end-diastolic volume, and hypertension to create a predictive model for MVD. A logistic regression model was created with an area under the receiver operating characteristics curve (AUC) of 0.825. To more specifically predict coronary three-vessel disease, the AUC was 0.847 when SSS, diabetes, and hypertension were selected. The mean probabilities of abnormality based on the MVD prediction model were 12%, 24%, 40%, and 51% for no-, one-, two-, and three-vessel disease, respectively ( p < 0.0001). For the model to select patients with stress-only imaging, the AUC was 0.78 when the model was created using SSS, stress end-systolic volume and the number of risk factors (diabetes, hypertension, chronic kidney disease, and a history of smoking).
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction.
- Record: found
- Abstract: not found
- Article: not found
Single Photon Emission Computed Tomography (SPECT) Myocardial Perfusion Imaging Guidelines: Instrumentation, Acquisition, Processing, and Interpretation

- Record: found
- Abstract: found
- Article: found