- Record: found
- Abstract: found
- Article: found
Current Evidence Regarding Biomarkers Used to Aid Postoperative Delirium Diagnosis in the Field of Cardiac Surgery—Review
Read this article at
Abstract
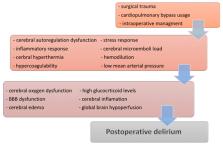
Postoperative cognitive disorders after cardiac surgery may manifest as postoperative delirium (POD) or later as postoperative cognitive dysfunction (POCD). The incidence of POD after cardiac surgery ranges from 16% to 73%. In contrast to POD, POCD is usually diagnosed after the discharge from hospital, with an incidence of 30 to 70% of cases, very often noticed only by close relative or friends, decreasing after six (20–30%) and twelve (15–25%) months after surgery. Perioperative cognitive disorders are associated with adverse short- and long-term effects, including increased morbidity and mortality. Due to the complexity of delirium pathomechanisms and the difficulties in the diagnosis, researchers have not yet found a clear answer to the question of which patient will be at a higher risk of developing delirium. The risk for POD and POCD in older patients with numerous comorbidities like hypertension, diabetes, and previous ischemic stroke is relatively high, and the predisposing cognitive profile for both conditions is important. The aim of this narrative review was to identify and describe biomarkers used in the diagnosis of delirium after cardiac surgery by presenting a search through studies regarding this subject, which have been published during the last ten years. The authors discussed brain-derived biomarkers, inflammation-related biomarkers, neurotransmitter-based biomarkers, and others. Work based on inflammation-related biomarkers, which are characterized by the low cost of implementation and the effectiveness of delirium diagnosis, seems to be the closest to the goal of discovering an inexpensive and effective marker. Currently, the use of a panel of tests, and not a single biomarker, brings us closer to the discovery of a test, or rather a set of tests ideal for the diagnosis of delirium after cardiac surgery.
Related collections
Most cited references119
- Record: found
- Abstract: found
- Article: not found
Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU
- Record: found
- Abstract: found
- Article: not found
Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression.
- Record: found
- Abstract: found
- Article: not found