- Record: found
- Abstract: found
- Article: found
A real-life study of the positive response to DAA-based therapies for hepatitis C in Brazil
Abstract
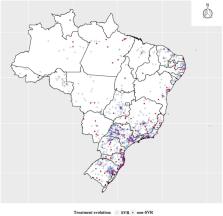
A retrospective cohort of 11,308 chronic hepatitis C infected patients treated with regimens that included Sofosbuvir (SOF), Daclatasvir (DCV), Simeprevir (SMV), or an association of Ombitasvir, Veruprevir/Ritonavir and Dasabuvir (3D) with or without Ribavirin (RBV) were assessed for sustained virologic response (SVR) or viral cure after a 12-week treatment. Logistic regression analyses were used to identify factors independently associated with positive response to direct-acting antivirals (DAA)-based therapies.
Overall 57.1% were male; 48.3% self-identified as white; 78.3% were over 50 years old; 44.1% were from the Southeast region; 47.7% had genotype 1b; and 84.5% were treated for 12 weeks. The SVR rates with DAAs ranged from 87% to 100%. Genotypes 1 and 4 had higher SVR rates (96.3–100%), and genotypes 2 and 3 had SVR of 90.6–92.2%, respectively. Treatment durations of 12 and 24 weeks were associated with an average SVR of 95.0% and 95.9%, respectively. Females were half as likely (OR 0.5; 95% CI 0.4−0.6) to have a negative response to therapy compared to males, and those with genotypes 2 and 3 were one and half fold more likely (OR 1.5–2.2; 95 CI% 0.7–2.9; 1.2–3.6 and OR 2.7–2.8; 95% CI 2.0–3.8, respectively) to not have SVR compared to genotype 1. Patients in the age-range of 50–69 years old were 1.2-fold (OR 1.2; 95% CI 0.7–1.9) more likely to not have SVR compared to other age groups, although not statistically significant.
This study is the first of this magnitude to be held in a Latin-American country with high SVR results, supported by a free-of-charge universal and public health system. The high performance found in this study gives support to the Brazilian public health policy decision of adopting DAA-based therapies as a strategy to eliminate HCV by 2030.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: found
Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study
- Record: found
- Abstract: found
- Article: not found
Orexin activation counteracts decreases in nonexercise activity thermogenesis (NEAT) caused by high-fat diet.
- Record: found
- Abstract: found
- Article: not found