- Record: found
- Abstract: found
- Article: found
Dendritic cell maturation in the corneal epithelium with onset of type 2 diabetes is associated with tumor necrosis factor receptor superfamily member 9
Read this article at
Abstract
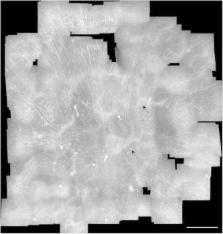
Type 2 diabetes mellitus is characterized by a low-grade inflammation; however, mechanisms leading to this inflammation in specific tissues are not well understood. The eye can be affected by diabetes; thus, we hypothesized that inflammatory changes in the eye may parallel the inflammation that develops with diabetes. Here, we developed a non-invasive means to monitor the status of inflammatory dendritic cell (DC) subsets in the corneal epithelium as a potential biomarker for the onset of inflammation in type 2 diabetes. In an age-matched cohort of 81 individuals with normal and impaired glucose tolerance and type 2 diabetes, DCs were quantified from wide-area maps of the corneal epithelial sub-basal plexus, obtained using clinical in vivo confocal microscopy (IVCM). With the onset of diabetes, the proportion of mature, antigen-presenting DCs increased and became organized in clusters. Out of 92 plasma proteins analysed in the cohort, tumor necrosis factor receptor super family member 9 (TNFRSF9) was associated with the observed maturation of DCs from an immature to mature antigen-presenting phenotype. A low-grade ocular surface inflammation observed in this study, where resident immature dendritic cells are transformed into mature antigen-presenting cells in the corneal epithelium, is a process putatively associated with TNFRSF9 signalling and may occur early in the development of type 2 diabetes. IVCM enables this process to be monitored non-invasively in the eye.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: not found
Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study.
- Record: found
- Abstract: found
- Article: not found
A central role for inflammation in the pathogenesis of diabetic retinopathy.
- Record: found
- Abstract: found
- Article: not found