- Record: found
- Abstract: found
- Article: found
Delayed diagnosis resulting in increased disease burden in multiple myeloma: the legacy of the COVID-19 pandemic
Read this article at
Abstract
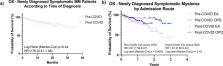
The COVID-19 pandemic has had global healthcare impacts, including high mortality from SARS-CoV-2 infection in cancer patients; individuals with multiple myeloma (MM) are especially susceptible to poor outcomes. However, even for MM patients who avoided severe infection, the ramifications of the pandemic have been considerable. The consequences of necessary socio-geographical behavior adaptation, including prolonged shielding and interruptions in delivery of non-pandemic medical services are yet to be fully understood. Using a real-world dataset of 323 consecutive newly diagnosed MM patients in England, we investigated the impact of the COVID-19 pandemic on routes to myeloma diagnosis, disease stage at presentation and relevant clinical outcomes. We demonstrate increasing MM presentations via emergency services and increased rates of bony and extra-medullary disease. Differences were seen in choice of induction therapy and the proportion of eligible patients undertaking autologous stem cell transplantation. Whilst survival was statistically inferior for emergency presentations, significant survival differences have yet to be demonstrated for the entire cohort diagnosed during the pandemic, making extended follow-up critical in this group. This dataset highlights wide-ranging issues facing MM patients consequent of the COVID-19 pandemic, with full impacts for clinicians and policy-makers yet to be elucidated.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma.

- Record: found
- Abstract: found
- Article: found
The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study

- Record: found
- Abstract: found
- Article: found