- Record: found
- Abstract: found
- Article: found
Burden of Neonatal Surgical Conditions in Northern Ghana
Read this article at
Abstract
Background
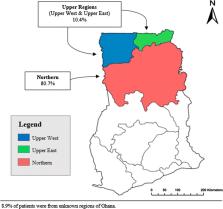
Congenital anomalies have risen to become the fifth leading cause of under-five mortality globally. The majority of deaths and disability occur in low- and middle-income countries including Ghana. This 3-year retrospective review aimed to define, for the first time, the characteristics and outcomes of neonatal surgical conditions in northern Ghana.
Methods
A retrospective study was conducted to include all admissions to the Tamale Teaching Hospital (TTH) neonatal intensive care unit (NICU) with surgical conditions between January 2014 and January 2017. Data were collected on demographics, diagnosis and outcomes. Descriptive analysis was performed on all data, and logistic regression was used to predict determinants of neonatal mortality. p < 0.05 was deemed significant.
Results
Three hundred and forty-seven neonates were included. Two hundred and sixty-one (75.2%) were aged 7 days or less at presentation, with males ( n = 177, 52%) slightly higher than females ( n = 165, 48%). The majority were delivered by spontaneous vaginal delivery ( n = 247, 88%); 191 (58%) were born in hospital. Congenital anomalies accounted for 302 (87%) of the neonatal surgical cases and 45 (96%) deaths. The most common anomalies were omphalocele ( n = 48, 13.8%), imperforate anus ( n = 34, 9.8%), intestinal obstruction ( n = 29, 8.4%), spina bifida ( n = 26, 7.5%) and hydrocephalus ( n = 19, 5.5%). The overall mortality rate was 13.5%. Two-thirds of the deaths ( n = 30) from congenital anomalies were conditions involving the digestive system with gastroschisis having the highest mortality of 88%. Omphalocele ( n = 11, 23.4%), gastroschisis ( n = 7, 14.9%) and imperforate anus ( n = 6, 12.8%) contributed to the most deaths. On multivariate analysis, low birthweight was significantly associated with mortality (OR 3.59, CI 1.4–9.5, p = 0.009).
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Congenital Anomalies in Low- and Middle-Income Countries: The Unborn Child of Global Surgery

- Record: found
- Abstract: found
- Article: found
Epidemiology of pediatric surgical needs in low-income countries
- Record: found
- Abstract: found
- Article: not found