- Record: found
- Abstract: found
- Article: found
Stereotactic Body Radiation Therapy Reirradiation for Locally Recurrent Rectal Cancer: Outcomes and Toxicity
Abstract
Purpose
Stereotactic body radiation therapy (SBRT) has emerged as a potential therapeutic option for locally recurrent rectal cancer (LRRC) but contemporaneous clinical data are limited. We aimed to evaluate the local control, toxicity, and survival outcomes in a cohort of patients previously treated with neoadjuvant pelvic radiation therapy for nonmetastatic locally recurrent rectal cancer, now treated with SBRT.
Methods and Materials
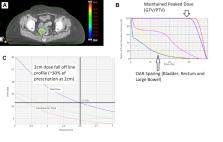
Inoperable rectal cancer patients with ≤3 sites of pelvic recurrence and >6 months since prior pelvic radiation therapy were identified from a prospective registry over 4 years. SBRT dose was 30 Gy in 5 fractions, daily or alternate days, using cumulative organ at risk dose constraints. Primary outcome was local control (LC). Secondary outcomes were progression free survival, overall survival, toxicity, and patient reported quality of life scores using the EQ visual analog scale (EQ-VAS) tool.
Results
Thirty patients (35 targets) were included. Median gross tumor volume size was 14.3 cm 3. In addition, 27 of 30 (90%) previously received 45 to 50.4 Gy in 25 of 28 fractions, with 10% receiving an alternative prescription. All patients received the planned reirradiation SBRT dose. The median follow-up was 24.5 months (interquartile range, 17.8-28.8). The 1-year LC was 84.9% (95% confidence interval [CI], 70.6-99) and a 2-year LC was 69% (95% CI, 51.8-91.9). The median progression free survival was 12.1 months (95% CI, 8.6-17.66), and median overall survival was 28.3 months (95% CI, 17.88-39.5 months). No patient experienced >G2 acute toxicity and only 1 patient experienced late G3 toxicity. Patient-reported QoL outcomes were improved at 3 months after SBRT (Δ EQ-VAS, +10 points, Wilcoxon signed-rank, P = .009).
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
RECIST 1.1-Update and clarification: From the RECIST committee.
- Record: found
- Abstract: found
- Article: not found
Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cancer on the basis of European randomized clinical trials.
- Record: found
- Abstract: found
- Article: not found